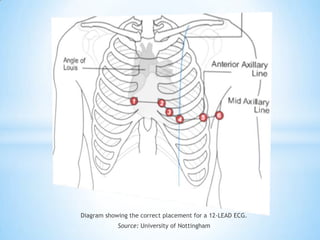
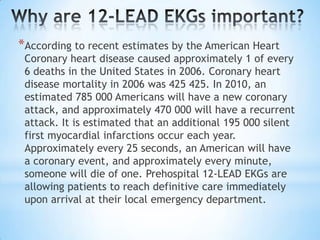
A 12-lead electrocardiogram (ECG) provides crucial information regarding the heart's electrical system and is commonly used for diagnosing acute coronary syndromes and dysrhythmias. Proper lead placement, preparation of the skin, and the patient's positioning are essential for accurate readings, along with immediate reporting of critical values observed in the ECG. The document highlights guidelines for conducting a 12-lead ECG, including electrode placement and maintenance, as well as the significance of timely and precise recording for patient care.