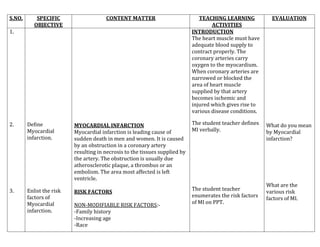
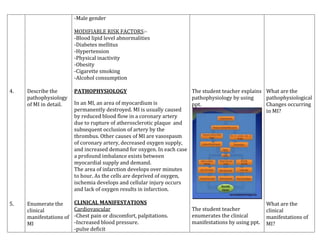
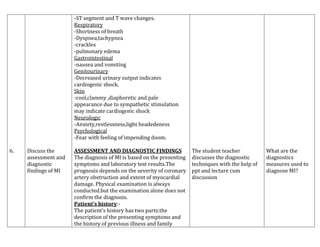
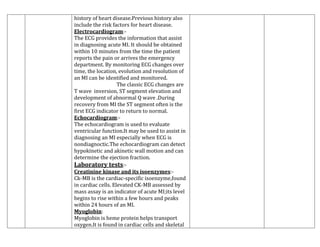
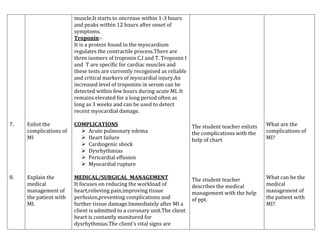
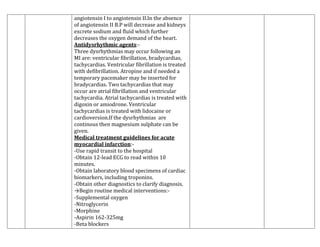
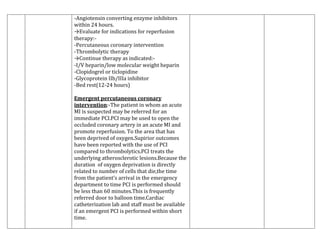
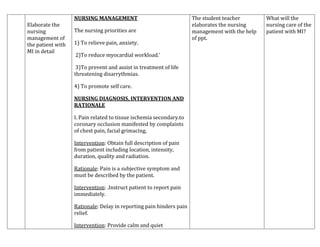
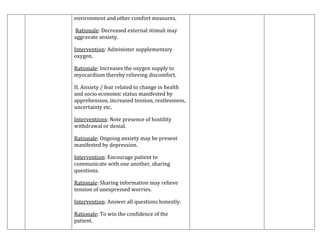
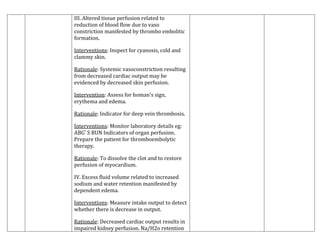
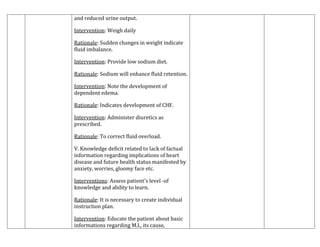
The document provides an extensive overview of myocardial infarction (MI), including its definition, risk factors, pathophysiology, clinical manifestations, diagnostic findings, medical management, and nursing strategies. It emphasizes the critical aspects of timely diagnosis and intervention, highlighting the importance of managing modifiable risk factors to prevent MI. Additionally, the document outlines various assessments and treatments to improve patient outcomes, making it a comprehensive guide for healthcare professionals dealing with MI.