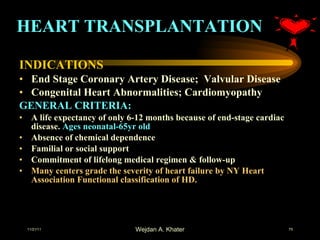
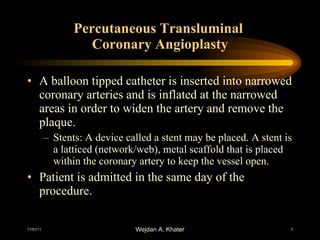
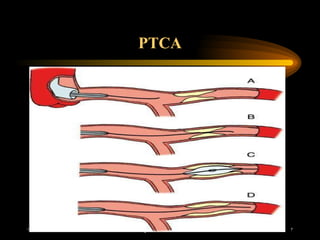
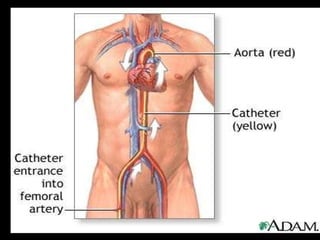
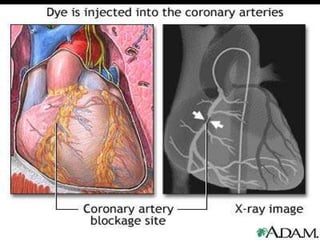
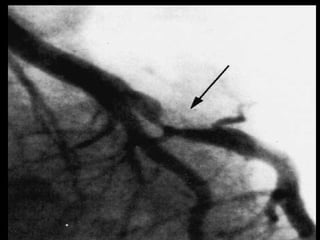
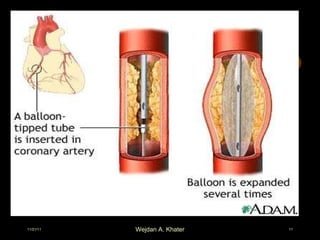
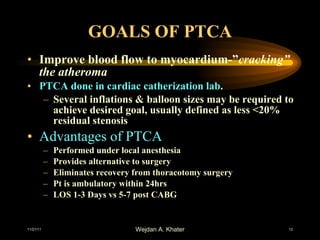
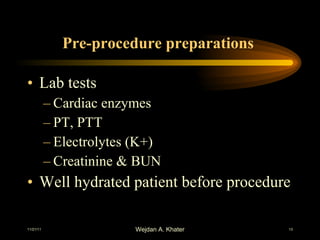
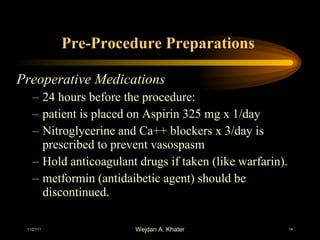
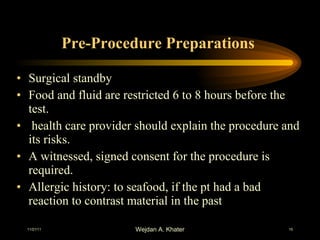
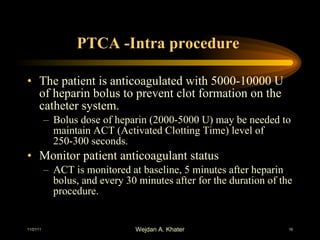
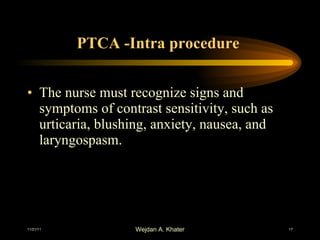
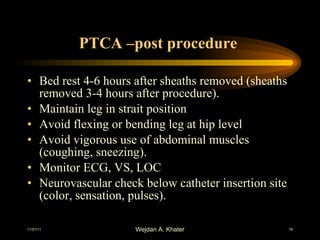
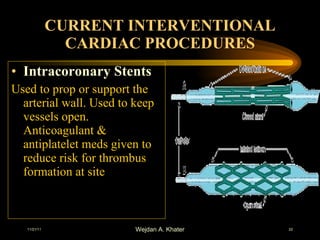
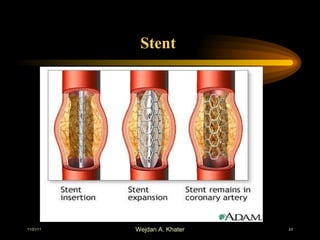
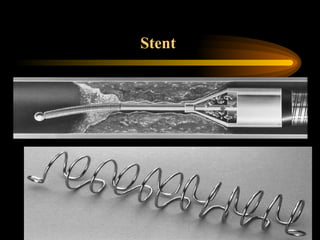
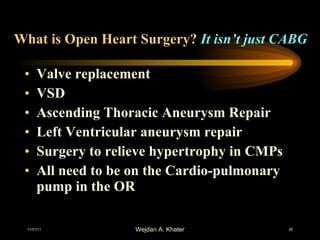
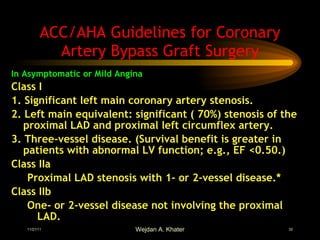
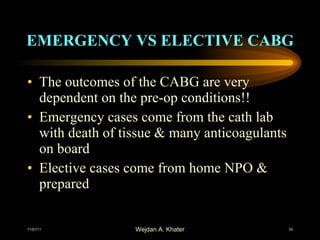
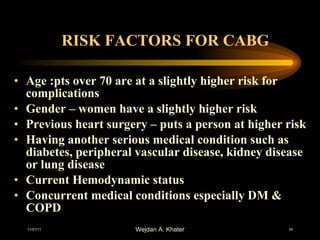
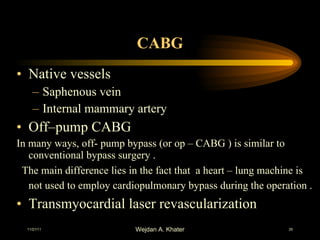
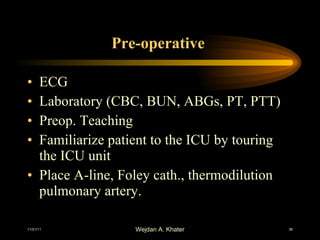
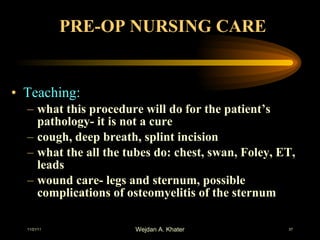
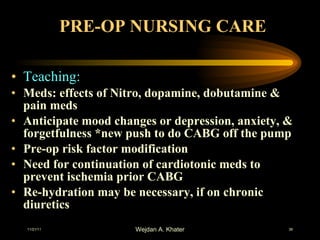
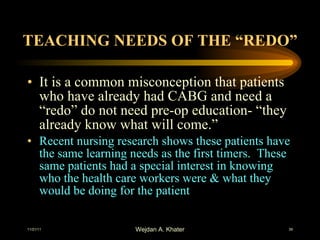
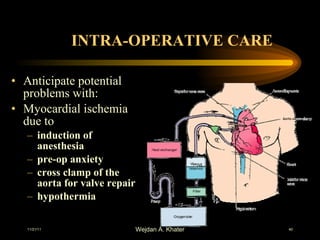
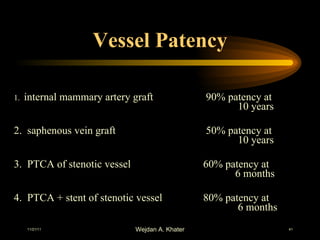
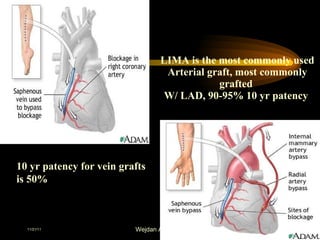
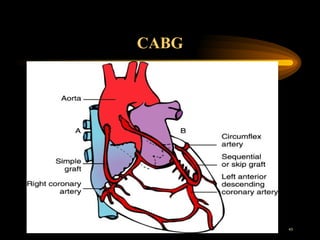
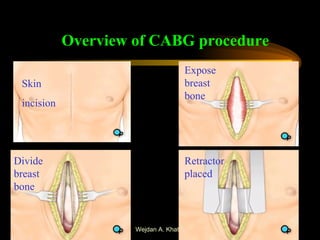
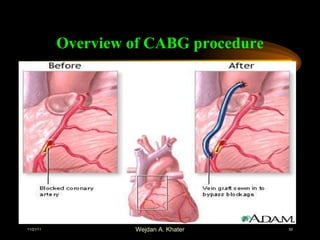
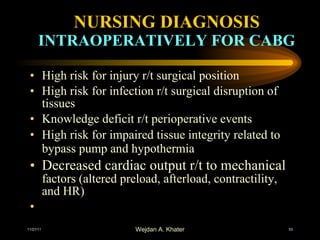
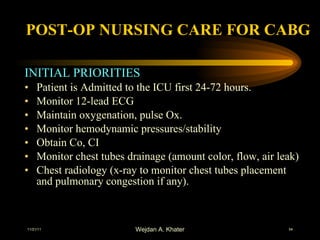
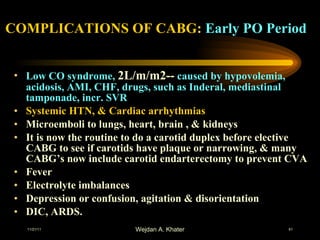
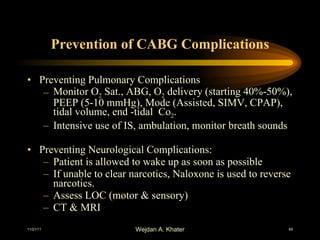
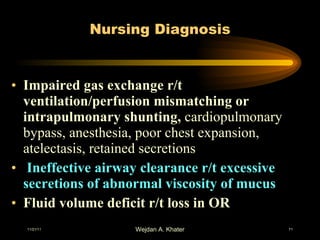
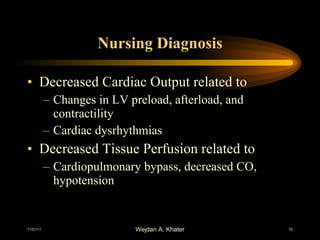
The document summarizes different cardiac procedures including percutaneous transluminal coronary angioplasty (PTCA), stenting, laser angioplasty, atherectomy, and coronary artery bypass grafting (CABG). PTCA involves inserting a balloon catheter into narrowed coronary arteries to widen them. Stents may be placed to keep arteries open. CABG is a surgical technique that uses leg veins or arteries to bypass blocked portions of coronary arteries. The document discusses indications, contraindications, pre-operative preparations, intraoperative and postoperative care for these procedures.

![Percutaneous Transluminal Coronary Angioplasty [PTCA] Indications for PTCA: Alleviate angina pectoris unrelieved by medical treatment Reduce the risk for MI Acute MI Persistent chest pain (angina) Pts with lesions >70% stenosis placing large areas of heart At risk for ischemia](https://image.slidesharecdn.com/cardiacsurgeryandptca-111121130012-phpapp01/85/Cardiac-surgery-and-ptca-4-320.jpg)
![Percutaneous Transluminal Coronary Angioplasty [PTCA] Indications for PTCA: Patients with surgical risk factors (elderly, poor LV Funx., sever underlying diseases). Blockage of one or more coronary arteries (Multivessel occlusion) Residual obstruction in a coronary artery during or after a heart attack Recurrent stenosis and graft closure of coronary disease for patients underwent CABG.](https://image.slidesharecdn.com/cardiacsurgeryandptca-111121130012-phpapp01/85/Cardiac-surgery-and-ptca-5-320.jpg)
![Percutaneous Transluminal Coronary Angioplasty [PTCA] CONTRAINDICATIONS Patients with left main CAD. Mild stenosis less than 50%](https://image.slidesharecdn.com/cardiacsurgeryandptca-111121130012-phpapp01/85/Cardiac-surgery-and-ptca-6-320.jpg)
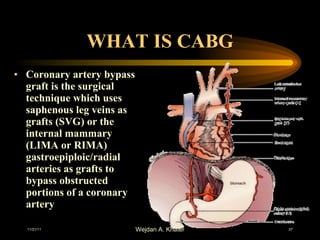
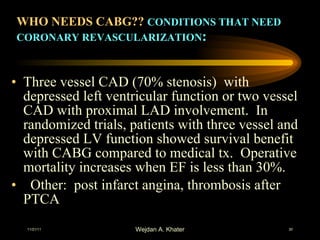
![WHO NEEDS CABG?? CONDITIONS THAT NEED CORONARY REVASCULARIZATION : Stable angina but meds not controlling pain, pt has function Non-successful PTCA with evolving MI Unstable angina A positive exercise tolerance test [treadmill], & lesions or blockage that cannot be treated by PTCA Exercise induced ventricular arrhythmias due to myocardial ischemia A Left Main Coronary lesion or blockage of more than 60% (50%) Single or double vessel disease with type B or C lesions](https://image.slidesharecdn.com/cardiacsurgeryandptca-111121130012-phpapp01/85/Cardiac-surgery-and-ptca-29-320.jpg)
![Complications of CABG: Late Postoperative Period Wound Infection Hepatitis Pancreatitis [early or late] Post-pericardiotomy syndrome Systemic arterial emboli & infective endocarditis, with valvular surgeries Occlusion of graft](https://image.slidesharecdn.com/cardiacsurgeryandptca-111121130012-phpapp01/85/Cardiac-surgery-and-ptca-65-320.jpg)
![Nursing Diagnosis Risk for infection r/t invasive catheter, surg. Wds. Acute pain r/t transmission and perception of cutaneous visceral, muscular, or ischemic pain [ Gerontological Consider.] Knowledge deficit r/t risk factor modification, discharge regime](https://image.slidesharecdn.com/cardiacsurgeryandptca-111121130012-phpapp01/85/Cardiac-surgery-and-ptca-73-320.jpg)