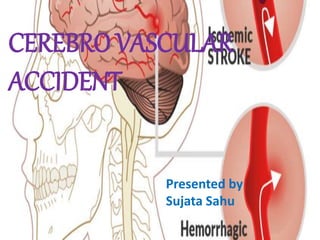
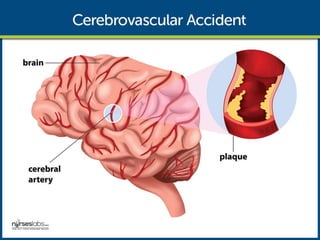
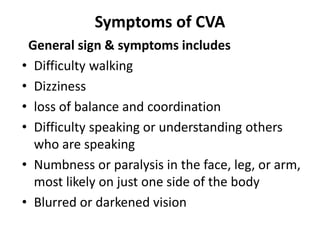
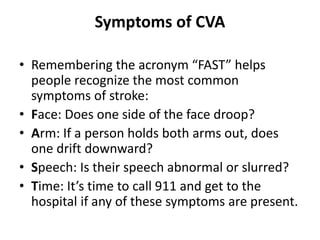
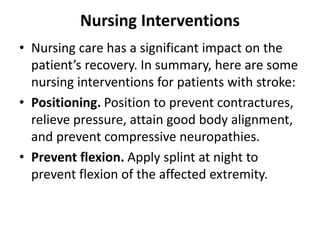
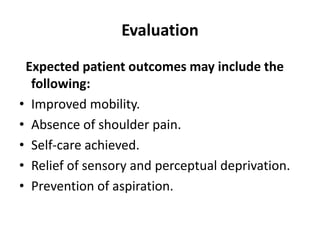
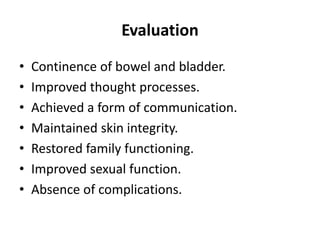
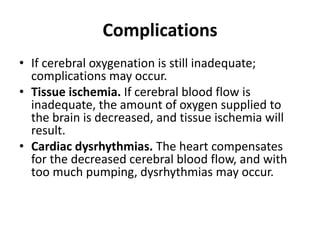
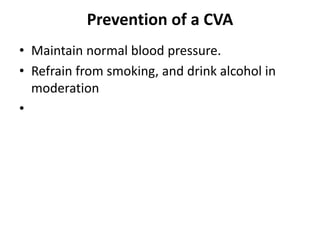
A cerebrovascular accident (CVA), also known as a stroke, is caused by disrupted blood flow to the brain resulting in the death of brain cells. There are two main types of strokes: ischemic strokes caused by blood clot blockages and hemorrhagic strokes caused by ruptured blood vessels. Treatment depends on the stroke type and may include clot-busting drugs, surgery, or controlling bleeding. Nursing care focuses on rehabilitation and prevention of complications through careful monitoring, positioning, and facilitating recovery of motor and cognitive functions. Lifestyle changes and medication can help prevent future strokes by managing risk factors like high blood pressure, smoking, obesity, and atrial fibrillation.