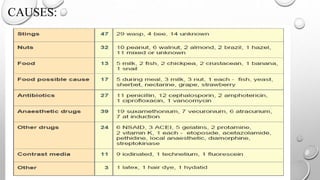
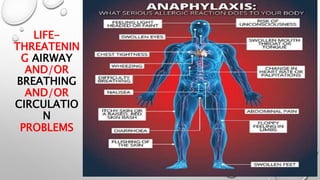
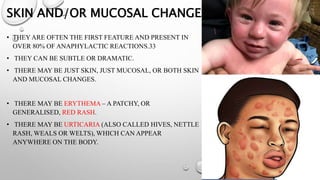
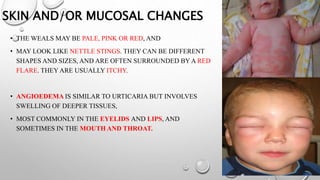
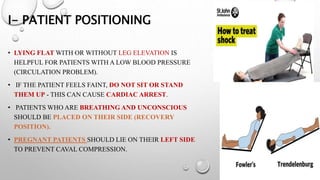
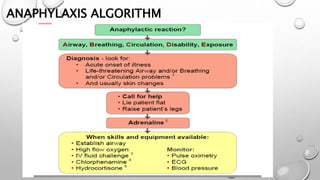
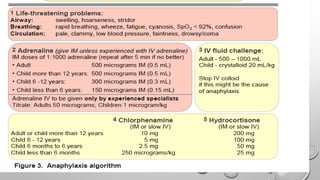
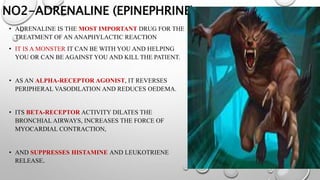
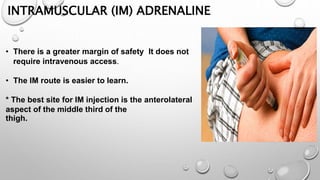
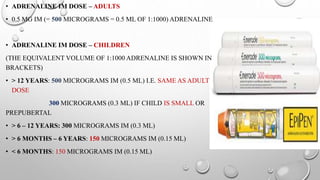
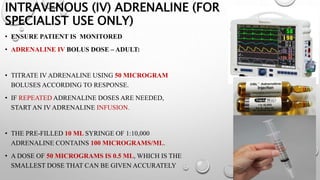
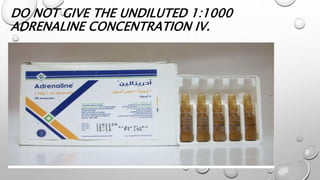
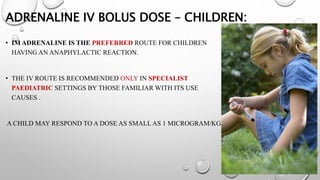
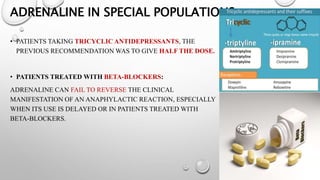
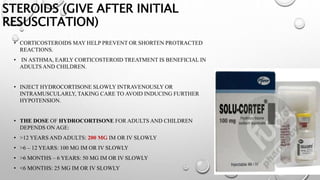
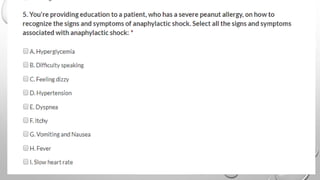
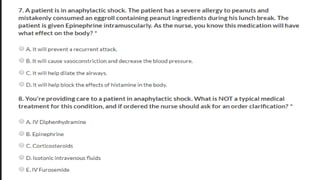
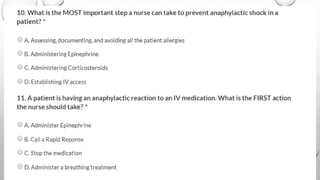
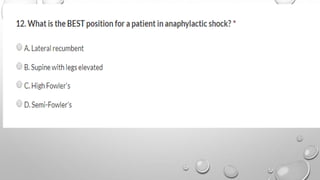
The document defines anaphylaxis as a severe, life-threatening generalized hypersensitivity reaction that is rapid in onset and involves airway, breathing, or circulatory problems along with skin and mucosal changes. It causes include foods, insects, medications, and latex. Fatal reactions typically cause respiratory arrest within 30-35 minutes for foods, collapse within 10-15 minutes for insect stings, and death within 5 minutes for intravenous medications. Symptoms involve various organ systems and progress rapidly. Treatment involves epinephrine, oxygen, fluids, antihistamines, steroids, and positioning the patient depending on their symptoms.