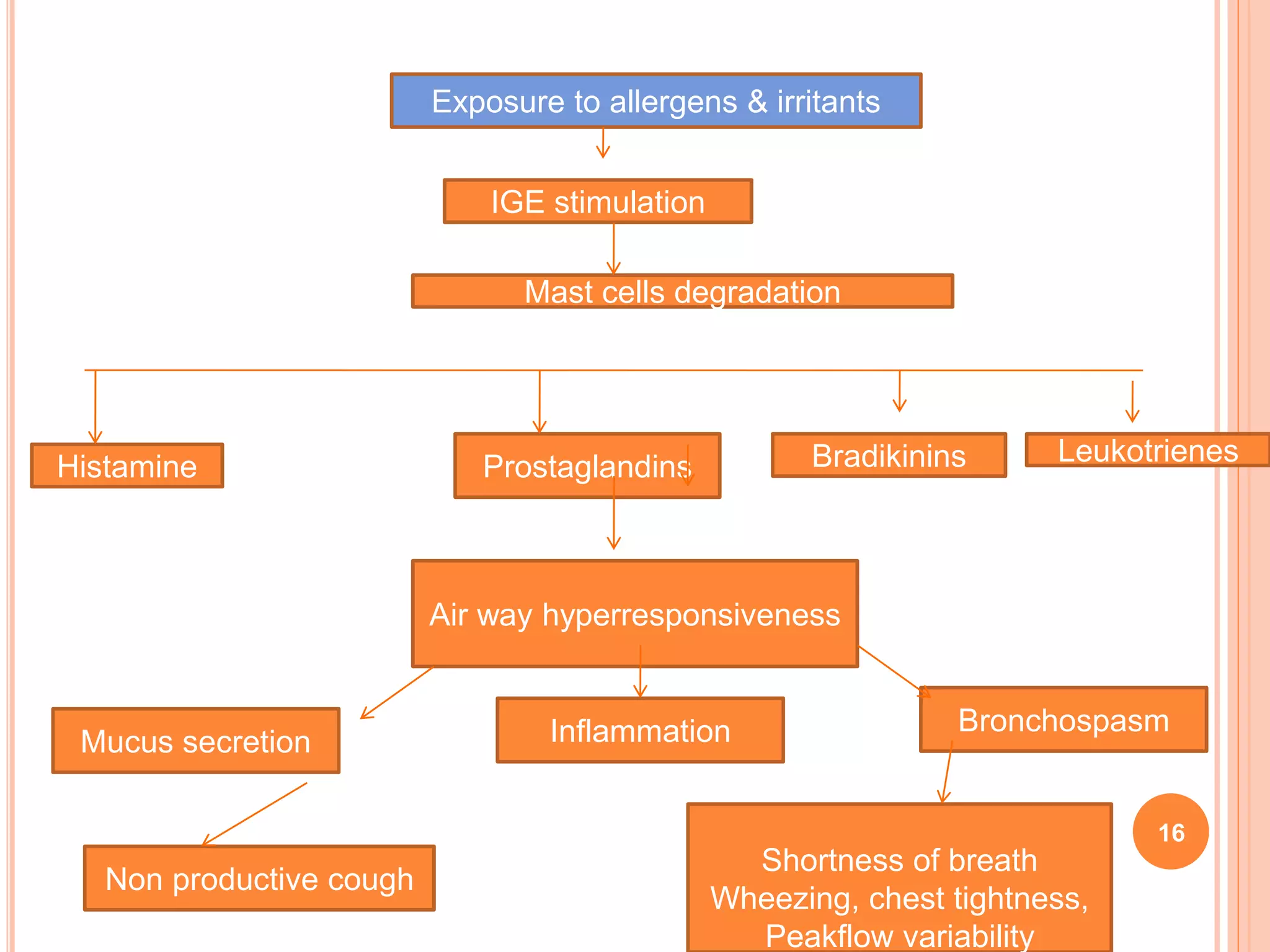
The document provides information on asthma, including its pathophysiology, epidemiology, risk factors, clinical manifestations, diagnosis, and treatment. Asthma is a chronic inflammatory disease of the airways characterized by airway hyperresponsiveness and reversible airflow obstruction. It commonly presents with wheezing, cough, chest tightness, and shortness of breath. Diagnosis involves assessing symptoms and lung function tests. Treatment focuses on reducing inflammation and managing acute exacerbations.