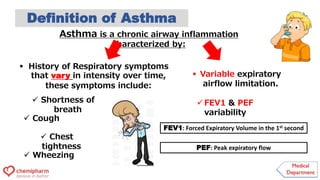
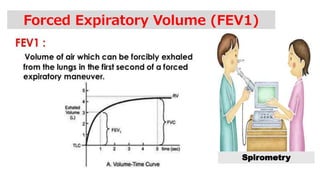
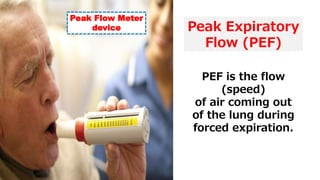
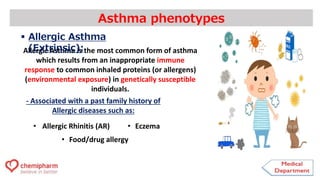
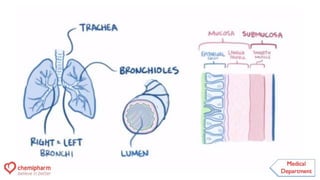
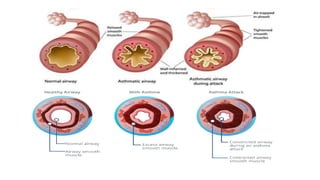
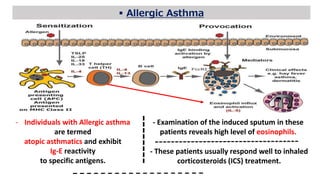
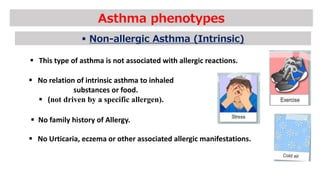
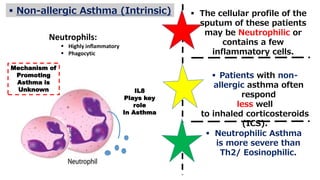
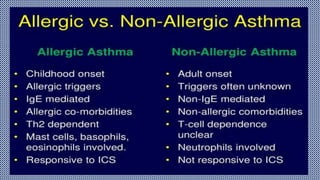
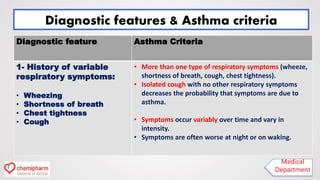
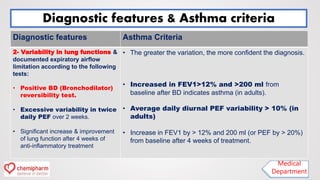
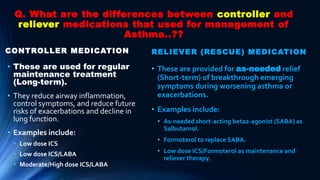
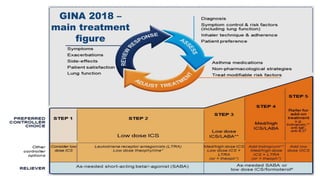
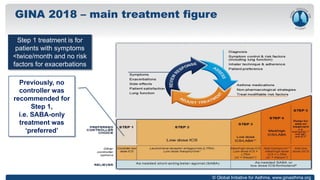
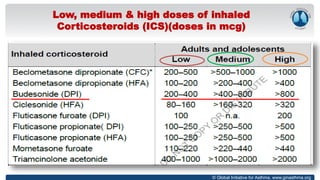
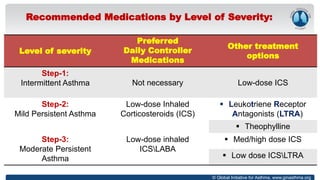
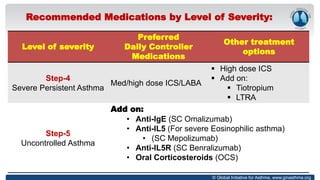
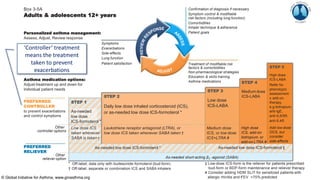
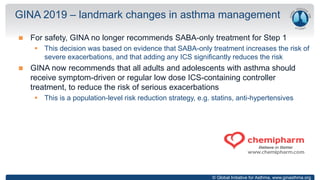
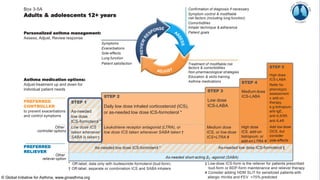
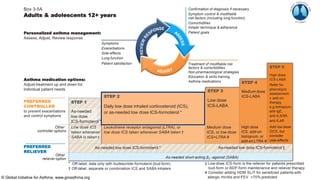
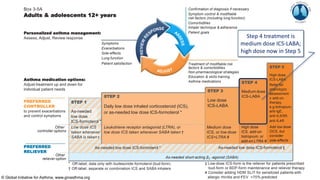
The document outlines updates in asthma management, detailing asthma as a chronic condition with variable respiratory symptoms and different phenotypes such as allergic and non-allergic asthma. It describes diagnostic criteria, including variability in lung function and the importance of inhaled corticosteroids (ICS) for treatment, emphasizing the revised Global Initiative for Asthma (GINA) management strategies. The treatment recommendations vary by severity, with a focus on personalized management and a shift away from short-acting beta2-agonist (SABA) only treatments to include ICS for better outcomes.