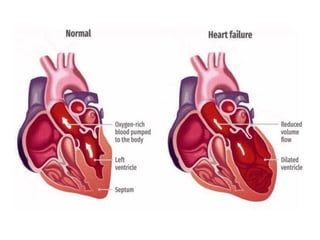
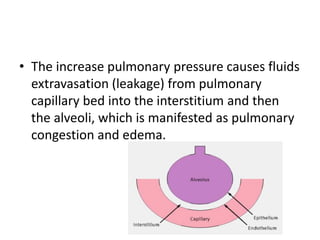
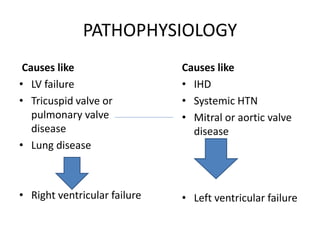
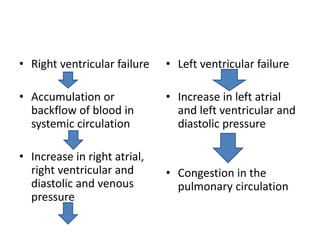
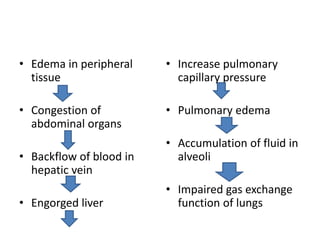
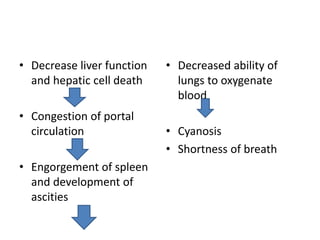
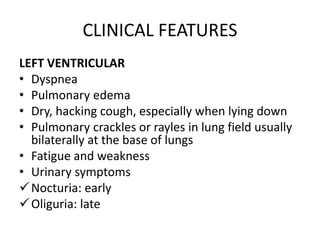
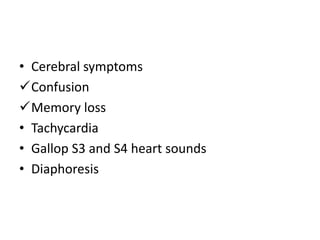
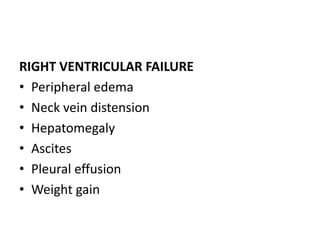
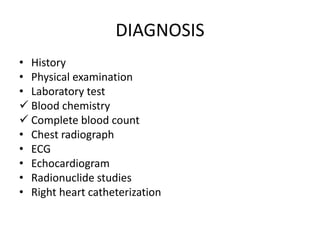
Congestive heart failure (CHF) is a syndrome characterized by the heart's inability to pump sufficient blood to meet the body's needs, resulting in impaired cardiac output and congestion. It can be classified into left-sided and right-sided failure, with left-sided failure being the most common form, leading to pulmonary congestion and edema, while right-sided failure causes systemic venous congestion. Diagnosis involves physical exams, lab tests, and imaging, with management including lifestyle modifications, pharmacological treatments, and potentially surgical interventions.