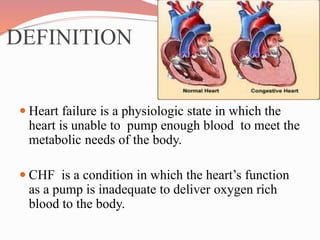
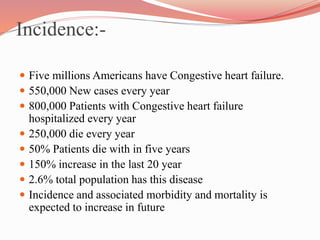
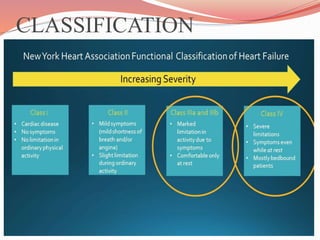
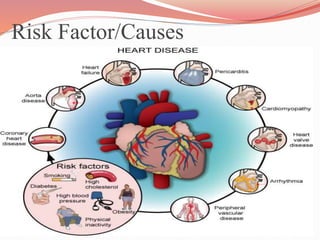
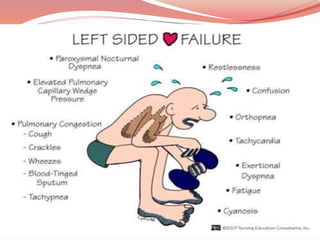
This document presents information on congestive heart failure. It begins with definitions of congestive heart failure and heart failure, noting that heart failure means the heart cannot pump enough blood to meet the body's needs. Statistics are provided on the incidence of congestive heart failure in the US, including that 800,000 patients are hospitalized annually and 250,000 die each year. The document discusses classifications, risk factors, signs and symptoms, diagnostic tests, pharmacological and surgical treatments, diet management, and nursing care for patients with congestive heart failure.