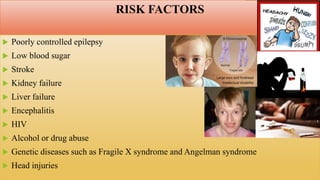
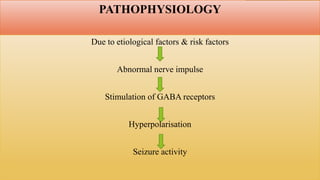
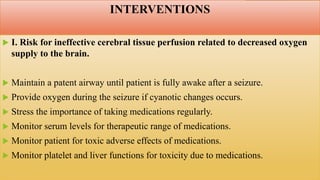
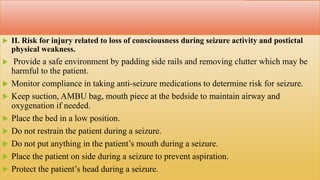
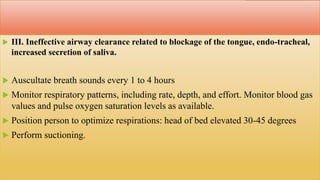
The document outlines the medical emergency known as status epilepticus, which is characterized by prolonged seizures exceeding 5 minutes or multiple seizures occurring within that time frame. It details the types of seizures, risk factors, clinical manifestations, diagnostic evaluations, and management strategies including both medical and nursing interventions. The goal is to maintain cerebral tissue perfusion, prevent injury, and promote self-health management among patients.