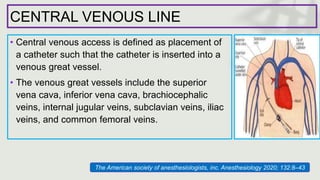
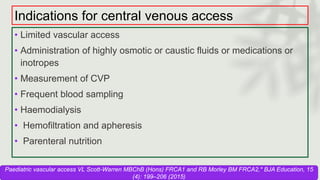
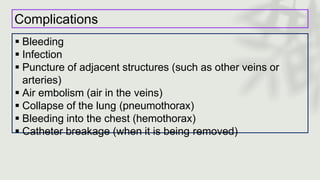
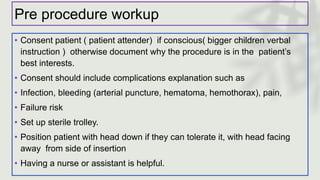
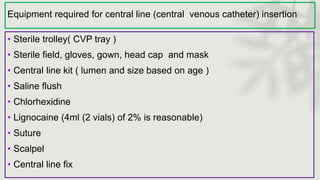
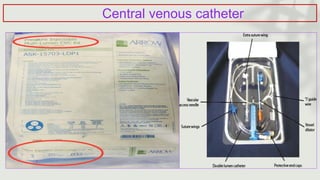
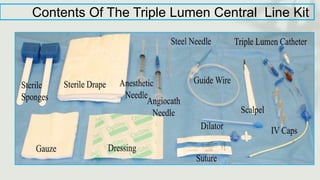
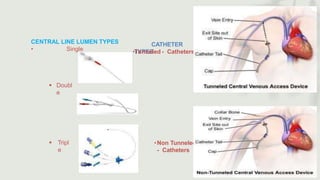
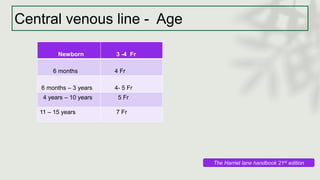
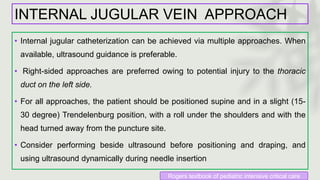
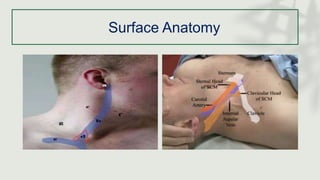
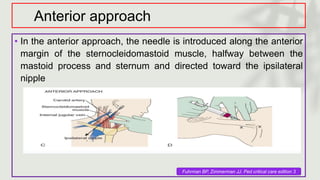
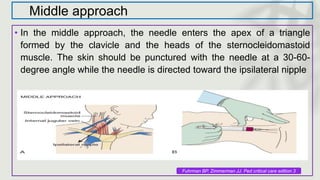
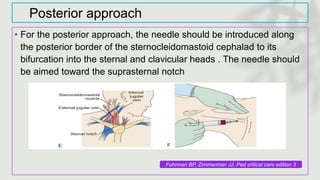
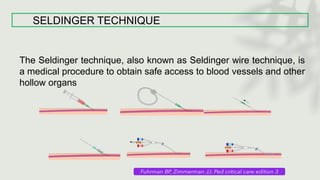
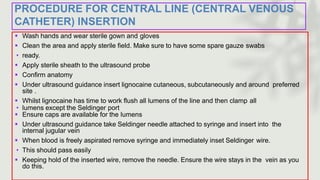
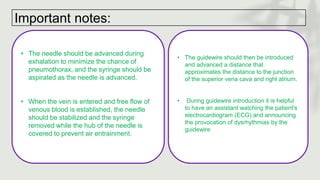
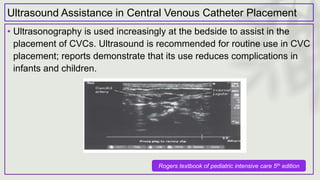
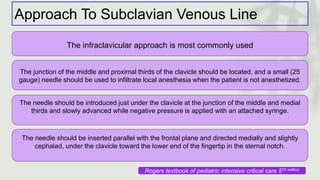
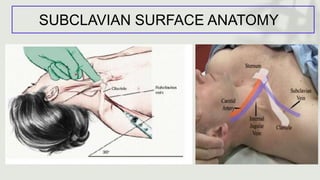
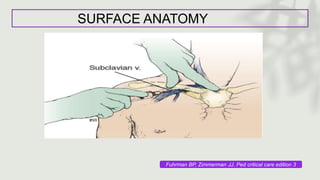
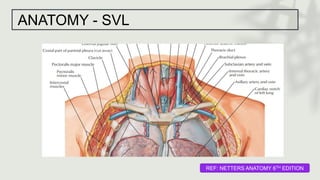
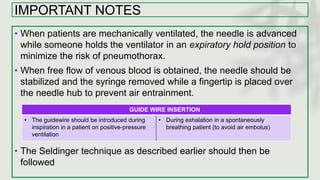
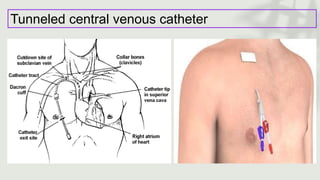
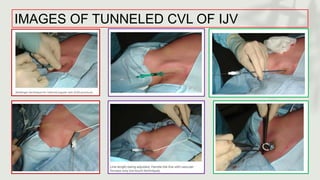
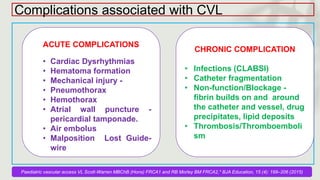
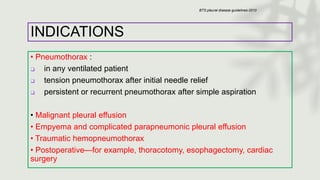
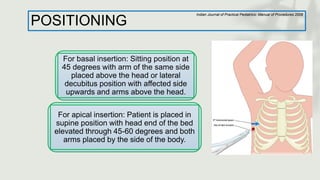
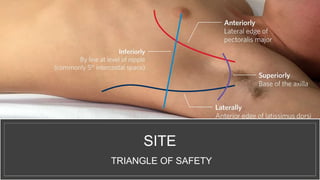
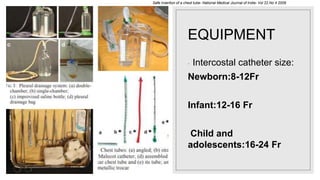
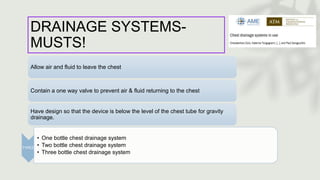
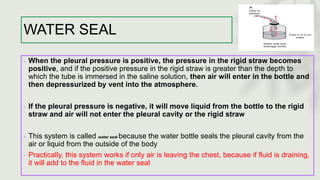
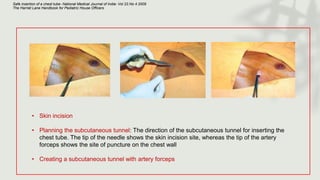
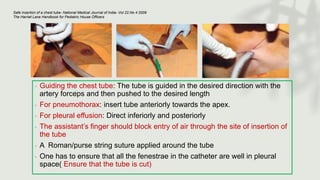
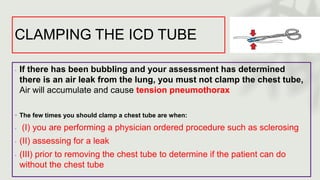
This document provides information on procedures in the pediatric intensive care unit (PICU) with a focus on central venous line insertion and intercostal drainage tube insertion. It discusses indications, contraindications, equipment, positioning, approaches and complications for central line placement via the internal jugular vein and subclavian vein. It also covers tunneled central venous catheters. For intercostal drainage, it reviews indications, contraindications, tube size, drainage systems, positioning, site selection and the basic procedure steps. Complications associated with both central lines and chest tubes are also summarized.