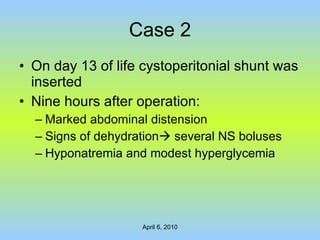
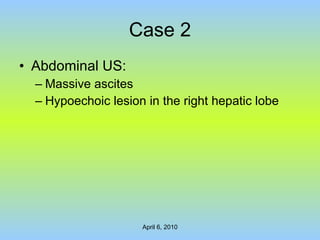
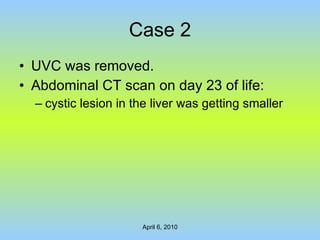
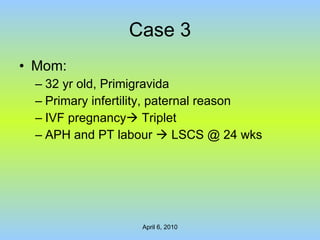
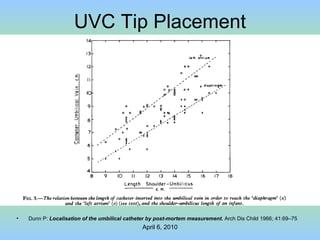
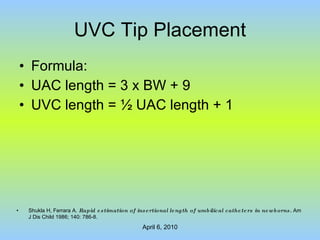
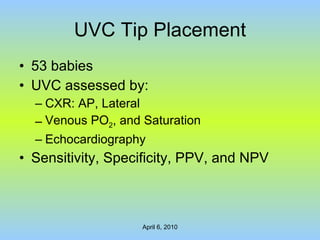
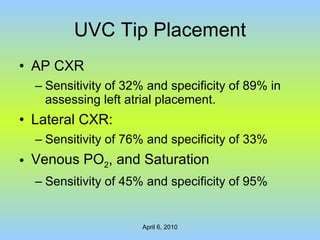
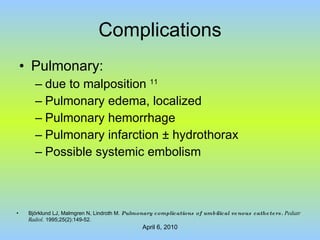
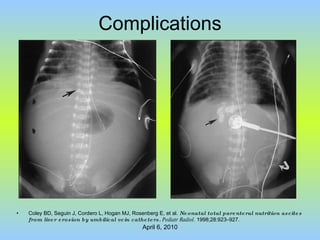
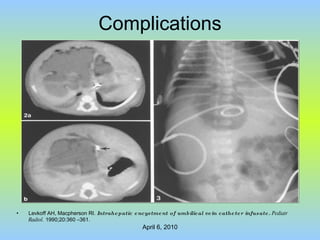
This document discusses umbilical venous catheters used in neonates, including three case studies. It outlines complications that can arise from malpositioning of the catheter tip, such as perforation of blood vessels, ascites, cardiac issues, and liver damage. Predicting the proper insertion length is difficult and radiography is not always reliable in confirming tip location. The recommendation is that further research is needed to determine the best length of insertion and that repeated imaging may help ensure the tip remains in the correct position.




























![Complications Recent study introduced a multimodal approach to reduce CR-BSI 17 : 15/1000 to 10/1000 catheter-days Sannoh S, Clones B, Munoz J, Montecalvo M, Parvez B. A multimodal approach to central venous catheter hub care can decrease catheter-related bloodstream infection . Am J Infect Control. 2010 Feb 3. [Epub ahead of print].](https://image.slidesharecdn.com/umbilicalvenouscatheter-100416214100-phpapp02/85/Umbilical-Venous-Catheter-46-320.jpg)