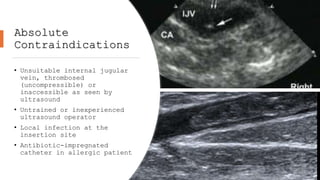
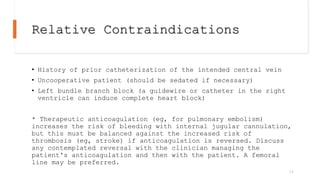
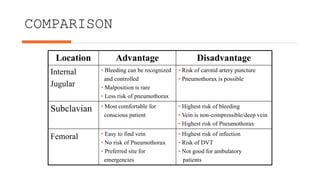
The document provides a comprehensive guide on internal jugular central venous access, covering its history, anatomy, indications, contraindications, complications, advantages, and equipment needed. It emphasizes that the internal jugular approach is preferred over subclavian and femoral due to lower risks of complications when ultrasound guidance is employed. It concludes by recommending the use of trained personnel and ultrasound for placement to maximize success rates and minimize risks.



![Relative Contraindications
• Coagulopathy, including therapeutic anticoagulation*
• Local anatomic distortion, traumatic or congenital, or gross
obesity
• Malignant superior vena cava syndrome
• Severe cardiorespiratory insufficiency or increased intracranial
or intraocular pressure (patients will be compromised by
Trendelenburg [head down] positioning)
13](https://image.slidesharecdn.com/tutorialkin-internaljugularcentralvenousaccess-240612012736-ae7879ab/85/Internal-Jugular-Central-Venous-Access-pptx-13-320.jpg)




![Seldinger (Catheter-over-
guidewire) Technique
• Cardiac monitor
• Local anesthetic (eg, 1%
lidocaine without
epinephrine, about 5 mL)
• Small anesthetic needle
(eg, 25 to 27 gauge,
about 1 inch [3 cm] long)
• Large anesthetic/finder*
needle (22 gauge, about
1.5 inches [4 cm] long)
• Introducer needle (eg,
thin-walled, 18 or 16
gauge, with internally
beveled hub, about 2.5
inches [6 cm] long)
• 3- and 5-mL syringes (use
slip-tip syringes for the
finder and introducer
needles)
• Guidewire, J-tipped
• Scalpel (#11 blade)
• Dilator
25](https://image.slidesharecdn.com/tutorialkin-internaljugularcentralvenousaccess-240612012736-ae7879ab/85/Internal-Jugular-Central-Venous-Access-pptx-25-320.jpg)
![Seldinger (Catheter-over-
guidewire) Technique
• Central venous catheter
(adult: 8 French or
larger, minimum length
for internal jugular
catheter is 15 cm for
right side, 20 cm for
left side)
• Sterile gauze (eg, 4 × 4
inch [10 × 10 cm]
squares)
• Sterile saline for
flushing catheter port or
ports
• Nonabsorbable nylon or
silk suture (eg, 3-0 or
4-0)
• Chlorhexidine patch,
transparent occlusive
dressing
A finder needle is a
thinner needle used for
locating the vein before
inserting the introducer
needle. It is usually not
needed for ultrasound-
guided cannulations.
The external diameter of
the CVC should be less
than or equal to one third
of the internal diameter
of the vein (as measured
by ultrasound) to reduce
the risk of thrombosis.
Having an assistant or two
is helpful.
26](https://image.slidesharecdn.com/tutorialkin-internaljugularcentralvenousaccess-240612012736-ae7879ab/85/Internal-Jugular-Central-Venous-Access-pptx-26-320.jpg)




![LIST OF
REFERENCE
S
• le Fevre, P. (n.d.). written and illustrated by
Central Venous Catheter Insertion Guide Central
Venous Catheter Insertion Guide About This Guide.
www.philippelefevre.com
• Mendenhall BR, Wilson C, Singh K, et al. Internal
Jugular Vein Central Venous Access. [Updated 2023
Aug 14]. In: StatPearls [Internet]. Treasure Island
(FL): StatPearls Publishing; 2024 Jan-. Available
from: https://www.ncbi.nlm.nih.gov/books/NBK436020/
• Central venous catheter insertion (Internal jugular
vein) - YouTube. (n.d.). Retrieved June 3, 2024,
from https://www.youtube.com/watch?v=O75D99DxWmM
• How To Do Internal Jugular Vein Cannulation,
Ultrasound-Guided - Critical Care Medicine - MSD
Manual Professional Edition. (n.d.). Retrieved June
3, 2024, from
https://www.msdmanuals.com/professional/critical-
care-medicine/how-to-do-central-vascular-
procedures/how-to-do-internal-jugular-vein-
cannulation,-ultrasound-guided
• Central Venous Catheters • LITFL Medical Blog • CCC.
(n.d.). Retrieved June 3, 2024, from
https://litfl.com/central-venous-catheters/
40](https://image.slidesharecdn.com/tutorialkin-internaljugularcentralvenousaccess-240612012736-ae7879ab/85/Internal-Jugular-Central-Venous-Access-pptx-40-320.jpg)
