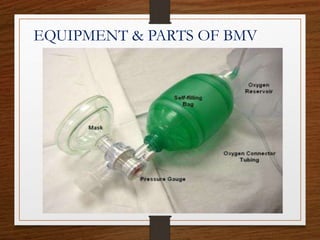
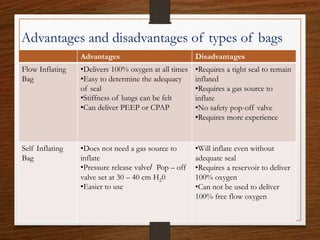
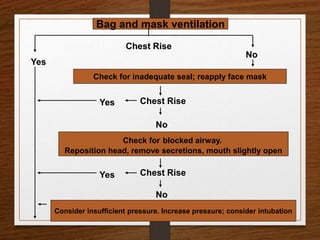
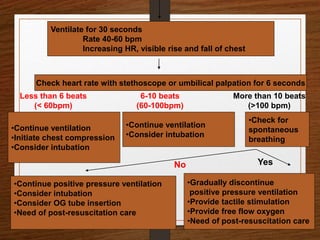
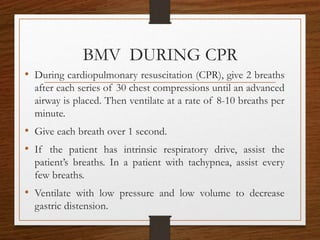
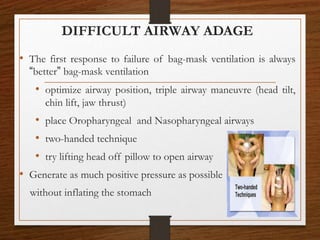
The document presents a comprehensive overview of bag and mask ventilation (BMV), highlighting its importance as a basic airway management technique, especially in pediatric patients. It covers the equipment and parts involved, types of bags, indications for use, procedural techniques, contraindications, complications, and nursing management. Additionally, it outlines the assessment for adequate ventilation and predictors of difficult airway scenarios, along with guidelines for handling complications and promoting respiratory function.