The document outlines various interventional procedures for central venous access in children, emphasizing proper techniques and anatomical considerations for safe catheter placement. It discusses indications for both central venous and intraosseous access, complications associated with these procedures, and the necessary equipment and techniques used in pediatric cases. Additionally, it covers umbilical vessel catheterization in neonates, including its uses, contraindications, and potential complications.
![Placement of central venous catheters
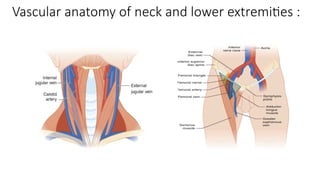
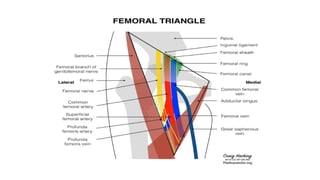
• The three most common anatomic locations for obtaining central
access in children are subclavian vein , the internal jugular vein and
femoral vein. The anatomic landmarks and insertion technique are
the same in adults and children
• The choice of location is depends on patient / children’s factor as well
as practitioner experience with particular site.
• Multiple attempts [>2] and the subclavian approach are associated
with higher complication rates.](https://image.slidesharecdn.com/interventionalprocedureinchildren-241109093740-51814ab8/85/INTERVENTIONAL-PROCEDURE-IN-CHILDREN-pptx-5-320.jpg)

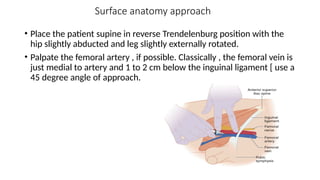
![• In pulseless arrest , locate the femoral vein using the “ v “ technique.
Place the thumb on pubic tubercle and the index finger on the
anterior superior iliac spine. Femoral vein is typically located at the
interdigital space [ the “ v “ of finger and thumb ] just inferior to
inguinal ligament.
• Always insert the needle below the inguinal ligament , because
vascular injury above the inguinal ligament may cause hemorhage
into retroperitoneal space.](https://image.slidesharecdn.com/interventionalprocedureinchildren-241109093740-51814ab8/85/INTERVENTIONAL-PROCEDURE-IN-CHILDREN-pptx-20-320.jpg)

![Complications of paediatric central venous access
• Pneumothorax / Haemothorax [ subclavian and internal jugular veins
sites]
• Thoracic duct injury [ left sided internal jugular vein]
• Arterial puncture
• Cardiac tamponade
• Air embolism
• Arrythmia
• Incorrect position
• Infections](https://image.slidesharecdn.com/interventionalprocedureinchildren-241109093740-51814ab8/85/INTERVENTIONAL-PROCEDURE-IN-CHILDREN-pptx-28-320.jpg)
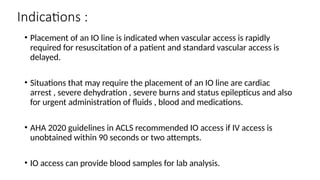
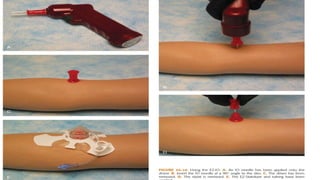
![Intraosseous [IO] vascular access
• IO vascular access is possible in patients of all ages when venous access
cannot be quickly and really established during circulatory collapse.
[ emergent need for vascular access ] and also alternative to central
venous access in pt without adequate peripheral access.
• Mechanical IO insertion devices have insertion time of only seconds
with consistently >90 % success rates.
• Insertion device include simple hand twist needles , hand held power
drills , spring loaded devices.
• Most common complication is extravasation at the insertion site.](https://image.slidesharecdn.com/interventionalprocedureinchildren-241109093740-51814ab8/85/INTERVENTIONAL-PROCEDURE-IN-CHILDREN-pptx-29-320.jpg)
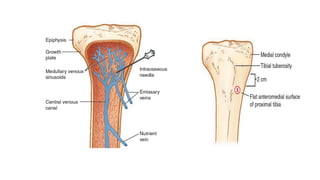
![Anatomy and pathophysiology :
• Long bones are composed of dense outer cortex and inner soft , spongy
[ cancellous ] bone.
• Nutrient artery supplies the bone with rich vascular network. It pierces the
cortex and divides into ascending and descending branches that further divided
into arterioles and capillaries.
• IO needle is inserted through cortex and into bone marrow [medullary] cavity of
a long bone.
• Most traditional site , which is favoured in paediatric patient , is the flat
anteromedial surface of proximal tibia.](https://image.slidesharecdn.com/interventionalprocedureinchildren-241109093740-51814ab8/85/INTERVENTIONAL-PROCEDURE-IN-CHILDREN-pptx-30-320.jpg)
![Contraindications to IO placement :
• Overlying infection
• Exposed bone
• underlying fracture
• Structural bone disorder [ eg. Osteogenesis imperfecta ]](https://image.slidesharecdn.com/interventionalprocedureinchildren-241109093740-51814ab8/85/INTERVENTIONAL-PROCEDURE-IN-CHILDREN-pptx-33-320.jpg)
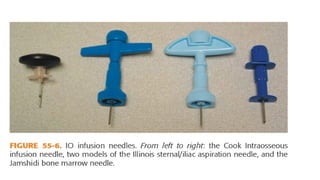
![IO cannulation devices :
• Two most common manual insertion devices include cook IO needle and
Jamshidi style IO needle.
• Powered devices are also available for IO needle insertion : examples are
EZ –IO and the Bone injection gun [ BIG ].
• Generally , powered IO devices in paediatrics are rapid to place with
minimal training , faster than manual devices and also felt to be easier to
use compared to other device.](https://image.slidesharecdn.com/interventionalprocedureinchildren-241109093740-51814ab8/85/INTERVENTIONAL-PROCEDURE-IN-CHILDREN-pptx-36-320.jpg)

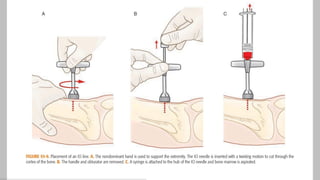

![Assessment :
• Assess whether the IO needle is correctly positioned within the
medullary cavity first aspirate the blood from marrow cavity may
not possible in patient with cardiac arrest [poor circulation ]
second sign of correct placement to assess whether the IO needle will
stand erect without support finally flush the IO line confirm
proper placement by ability of fluid to flow without inducing soft
tissue swelling.
• Ultrasonic visualization of flow within medullary cavity using color
doppler also confirm proper placement.](https://image.slidesharecdn.com/interventionalprocedureinchildren-241109093740-51814ab8/85/INTERVENTIONAL-PROCEDURE-IN-CHILDREN-pptx-44-320.jpg)