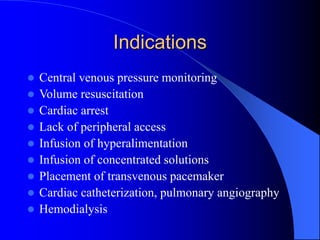
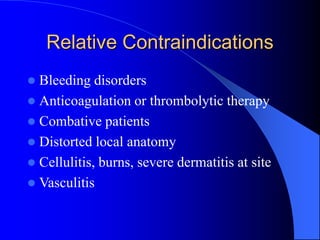
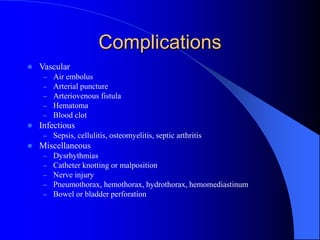
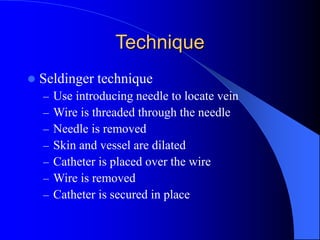
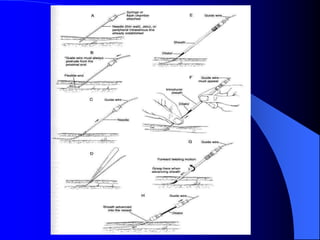
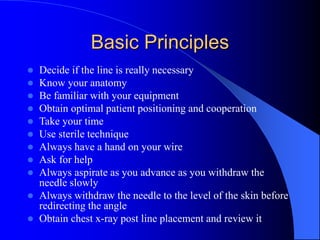
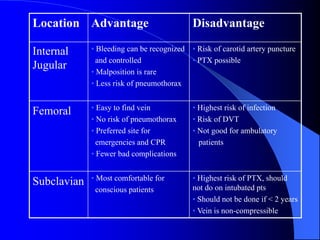
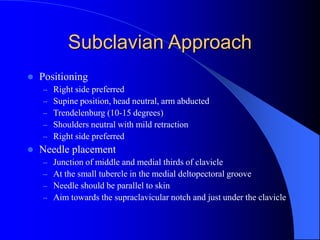
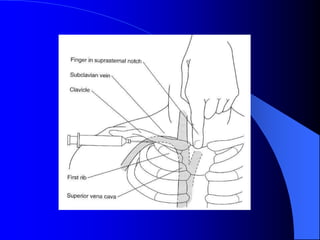
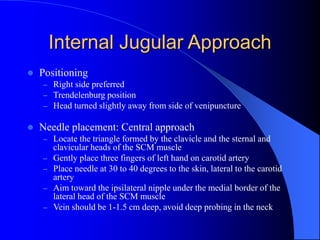
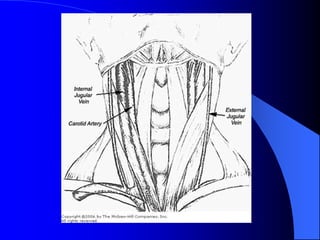
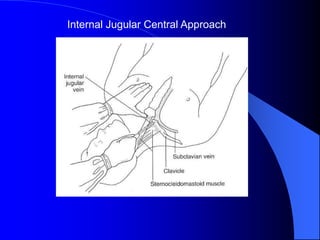
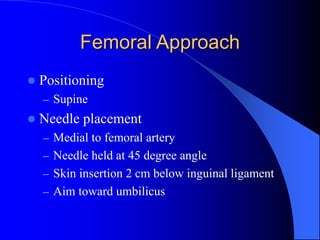
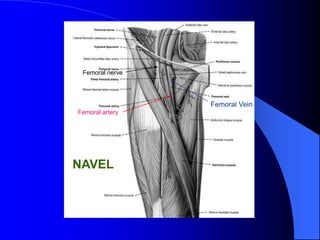
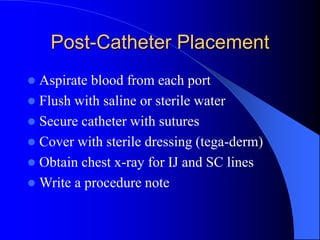
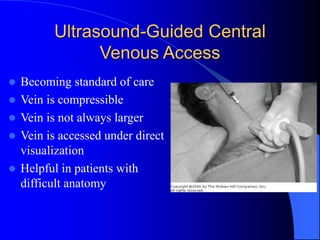
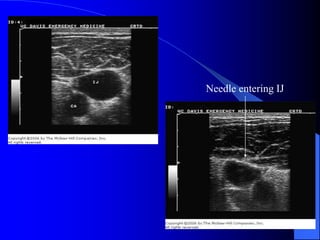
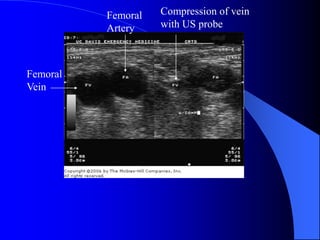
This document provides information on central venous catheterization including indications, contraindications, complications, technique, tips, and materials. It discusses the Seldinger technique for placement and reviews approaches for the internal jugular, subclavian, and femoral veins. Ultrasound guidance is becoming standard to help with difficult access and visualize the vein and needle. Proper technique and awareness of anatomy, complications, and indications can help ensure safe central line placement.