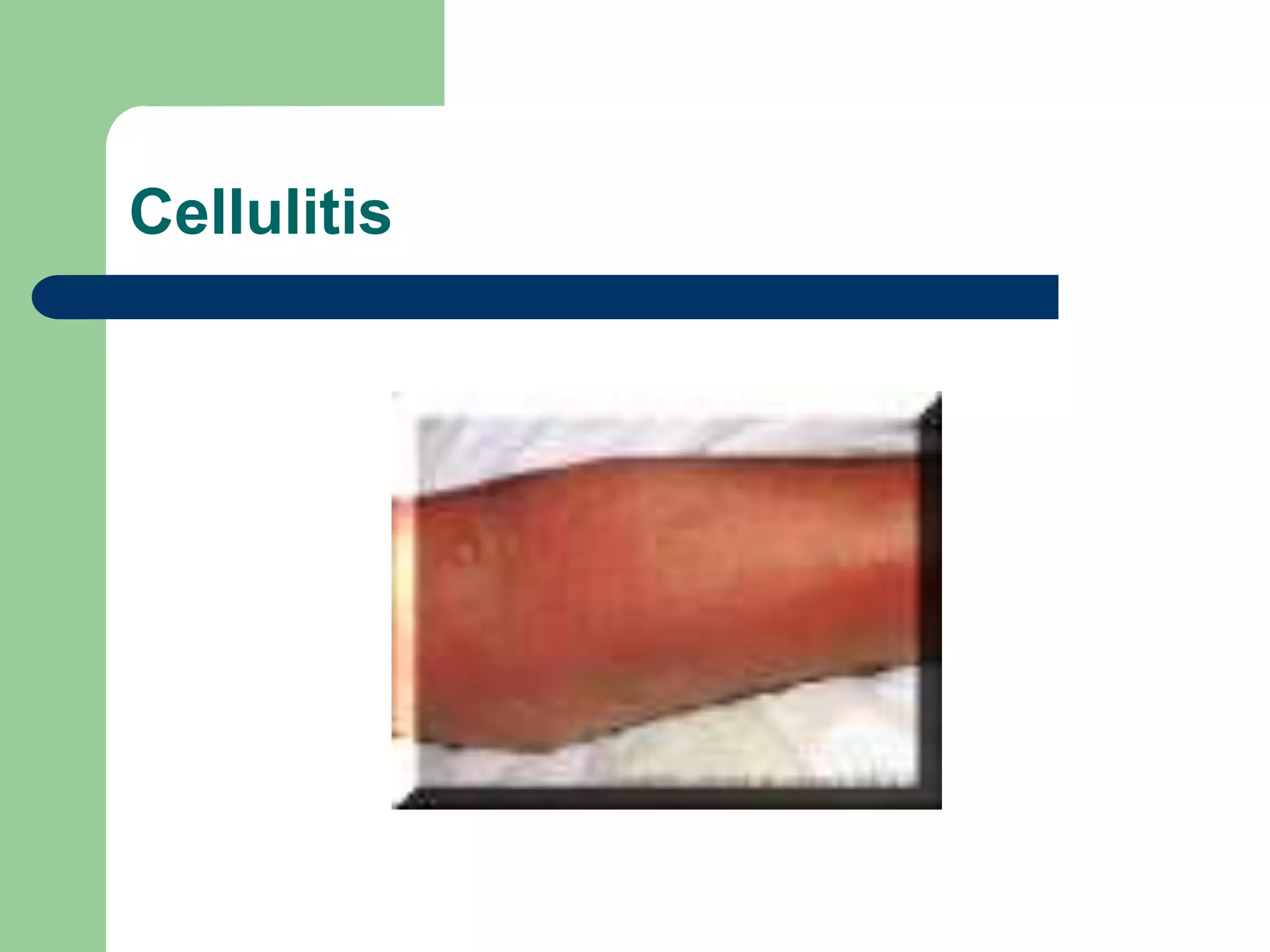
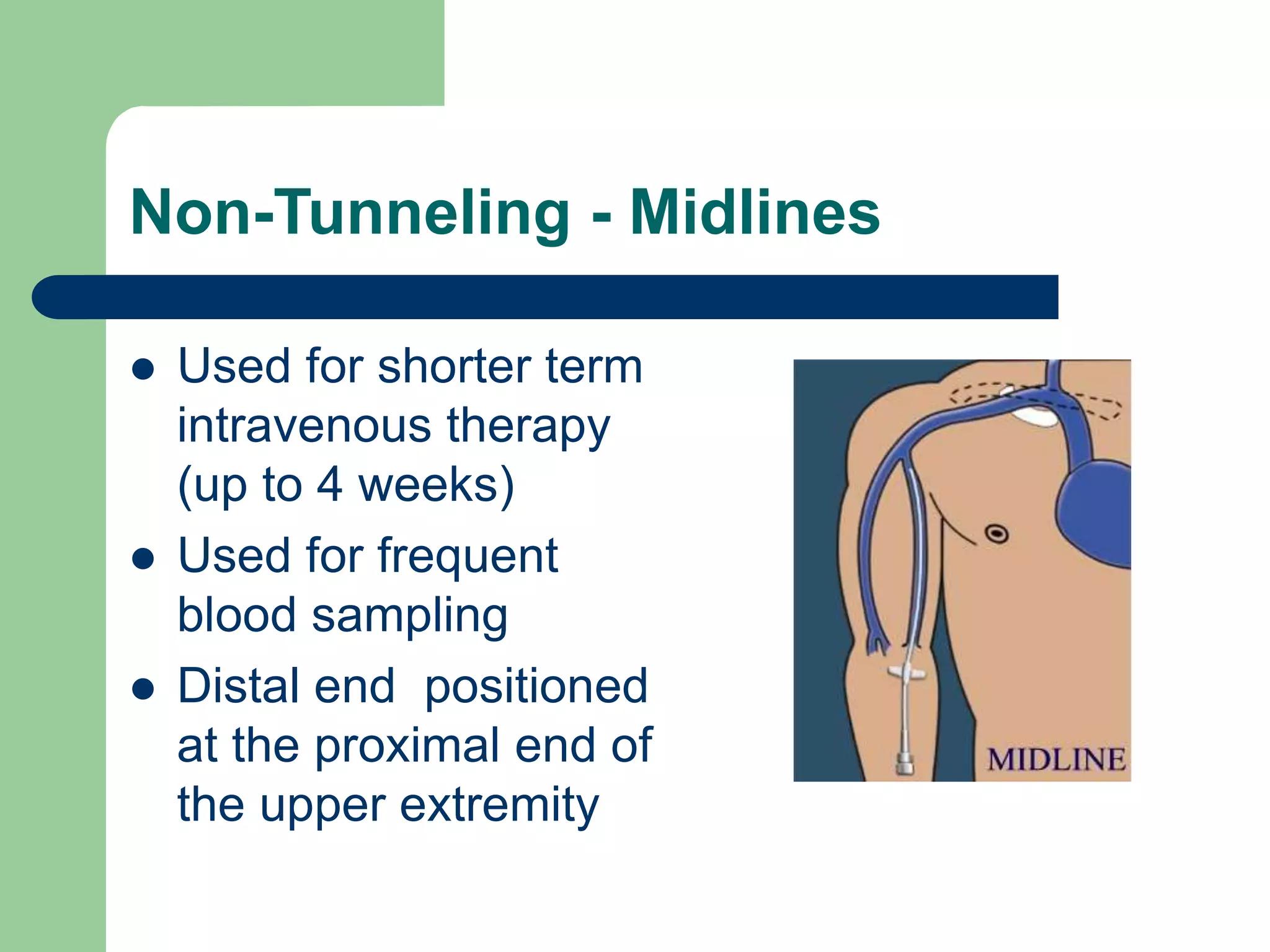
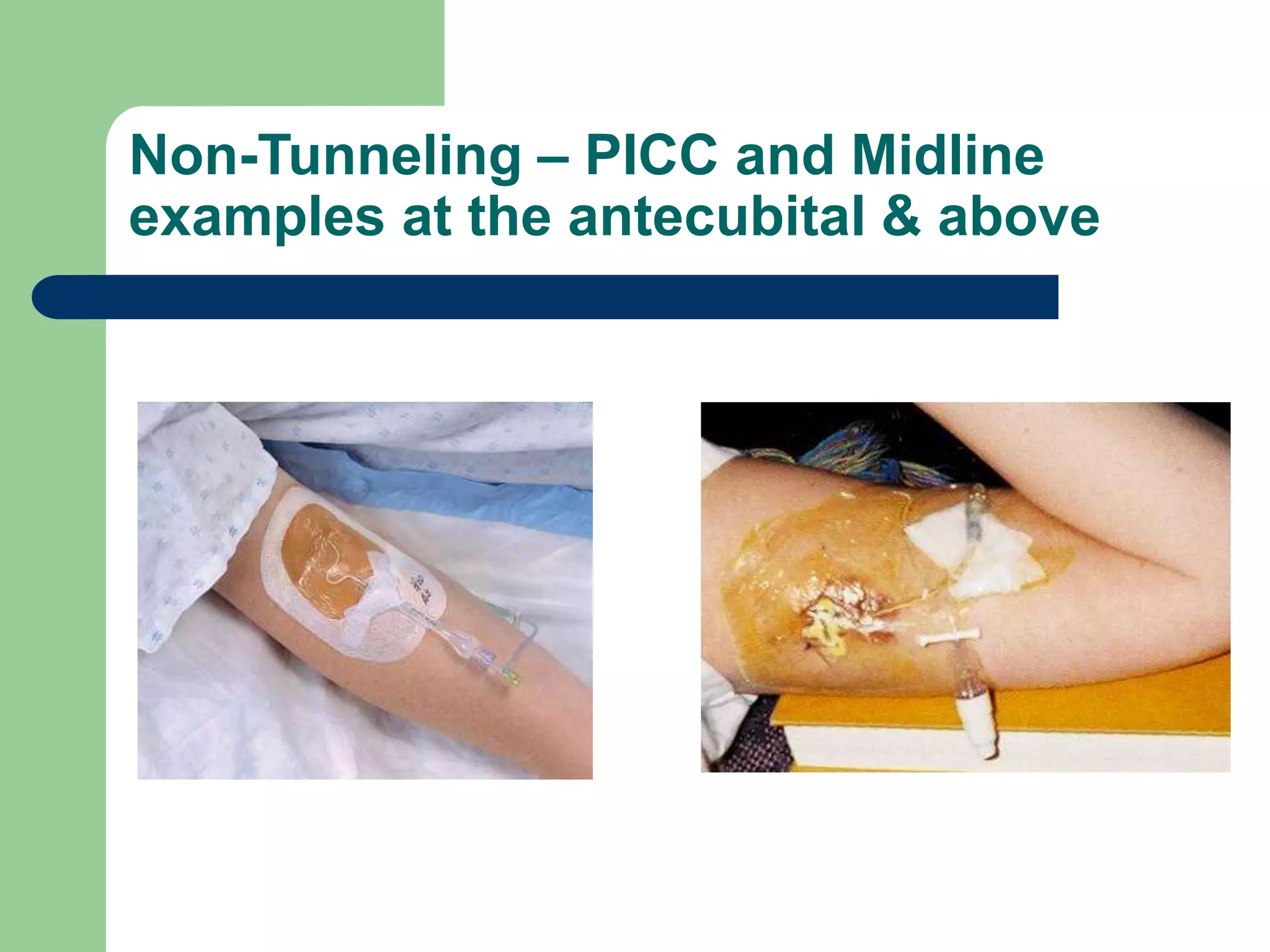
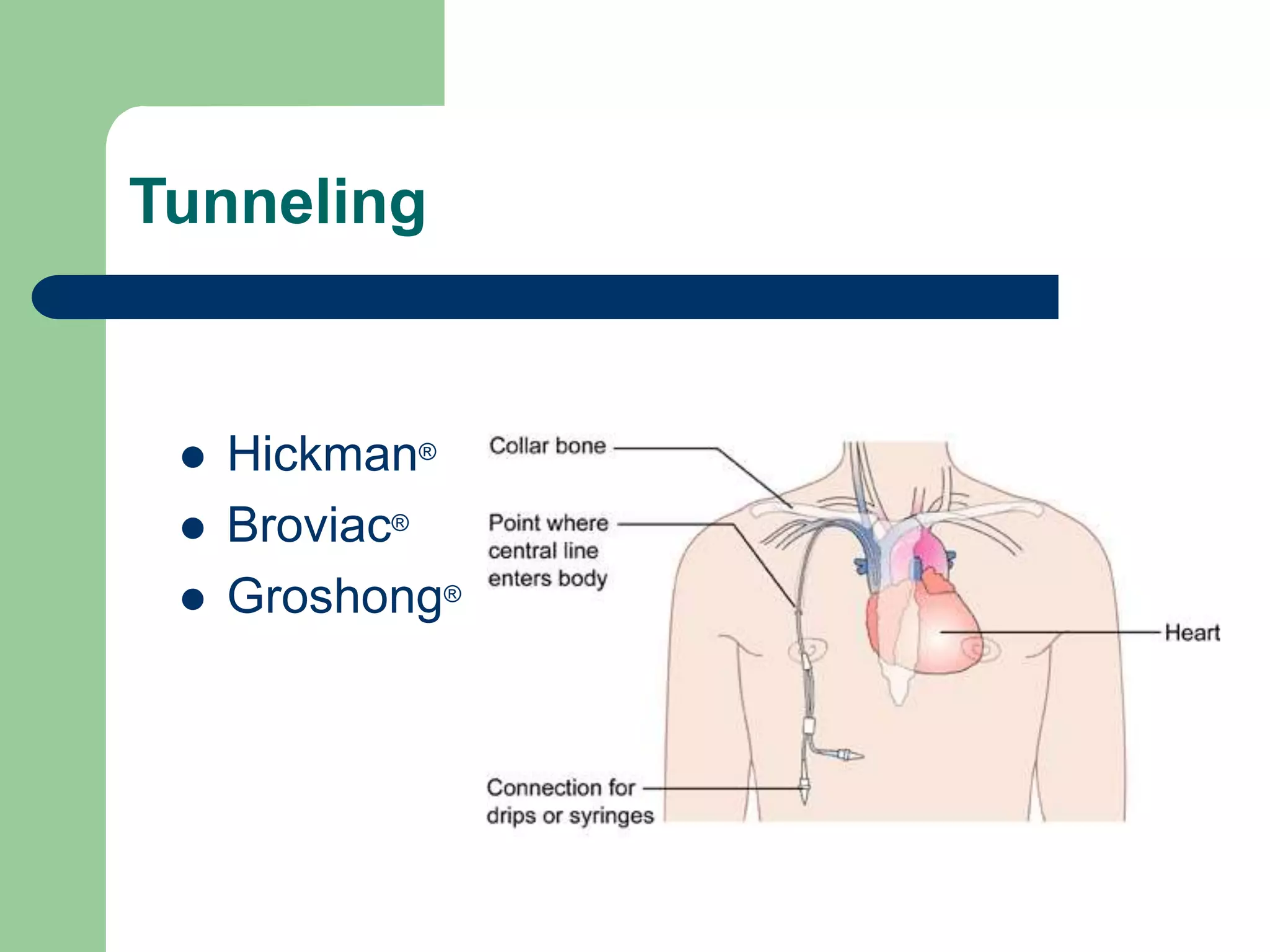
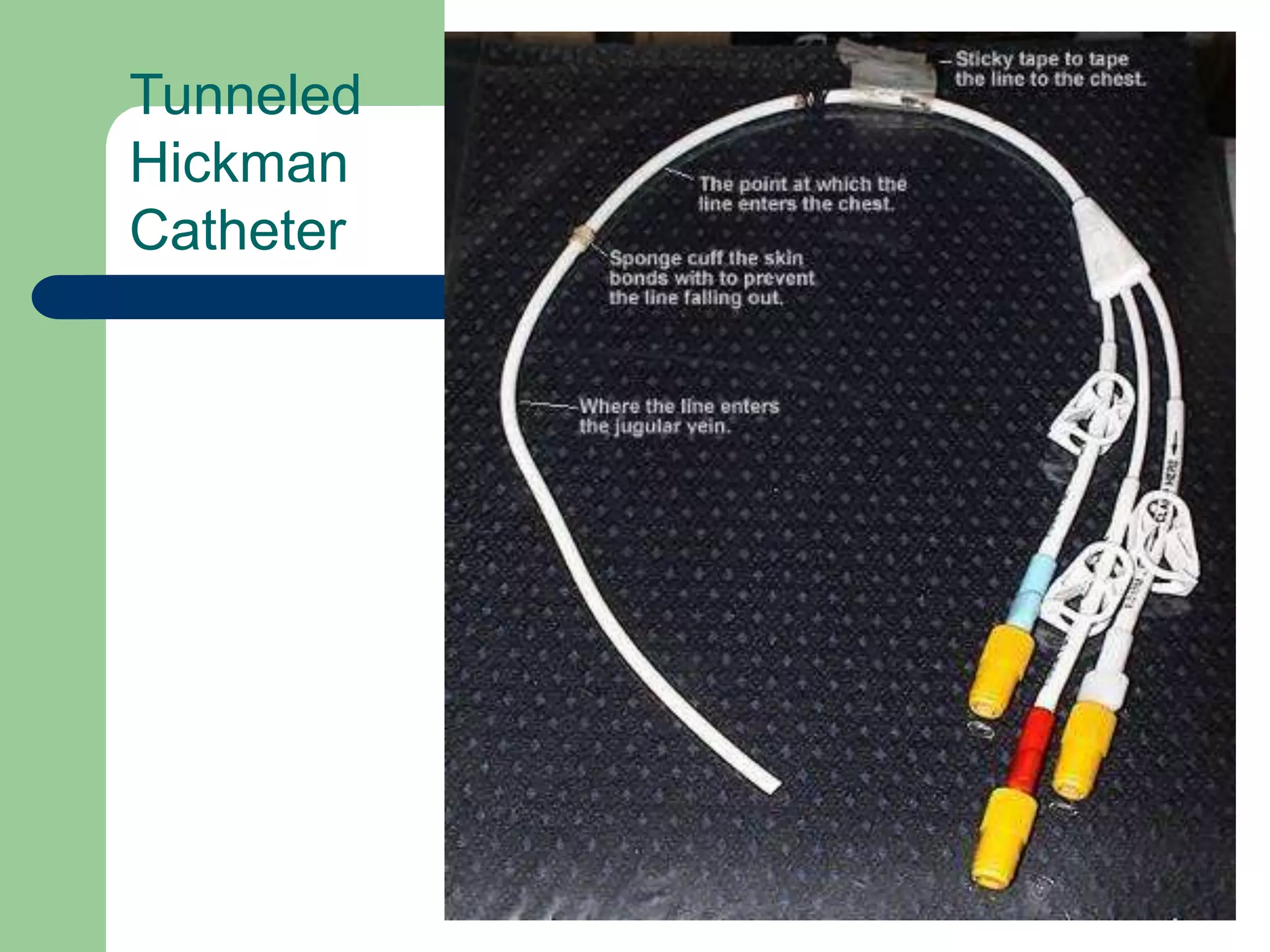
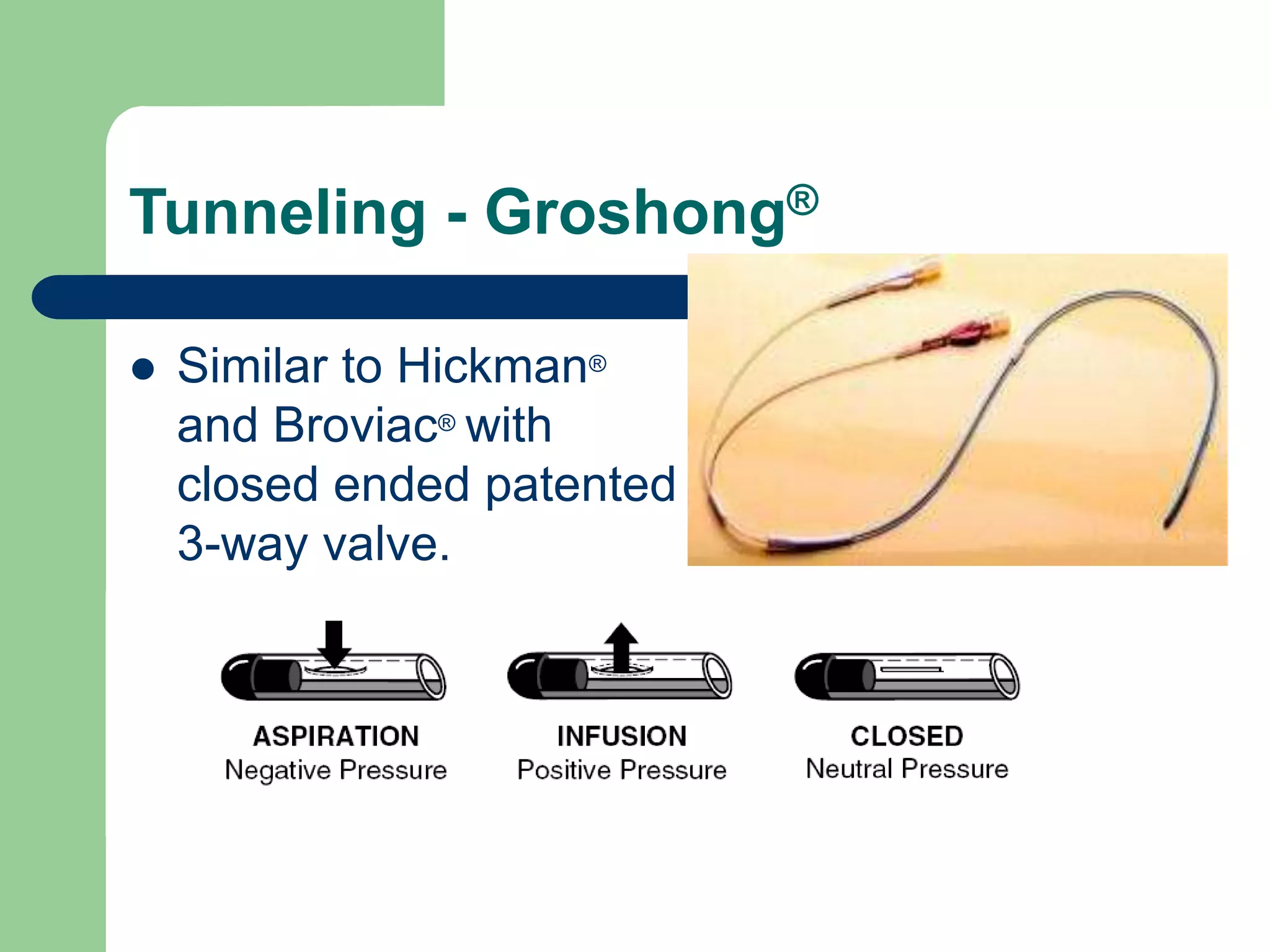
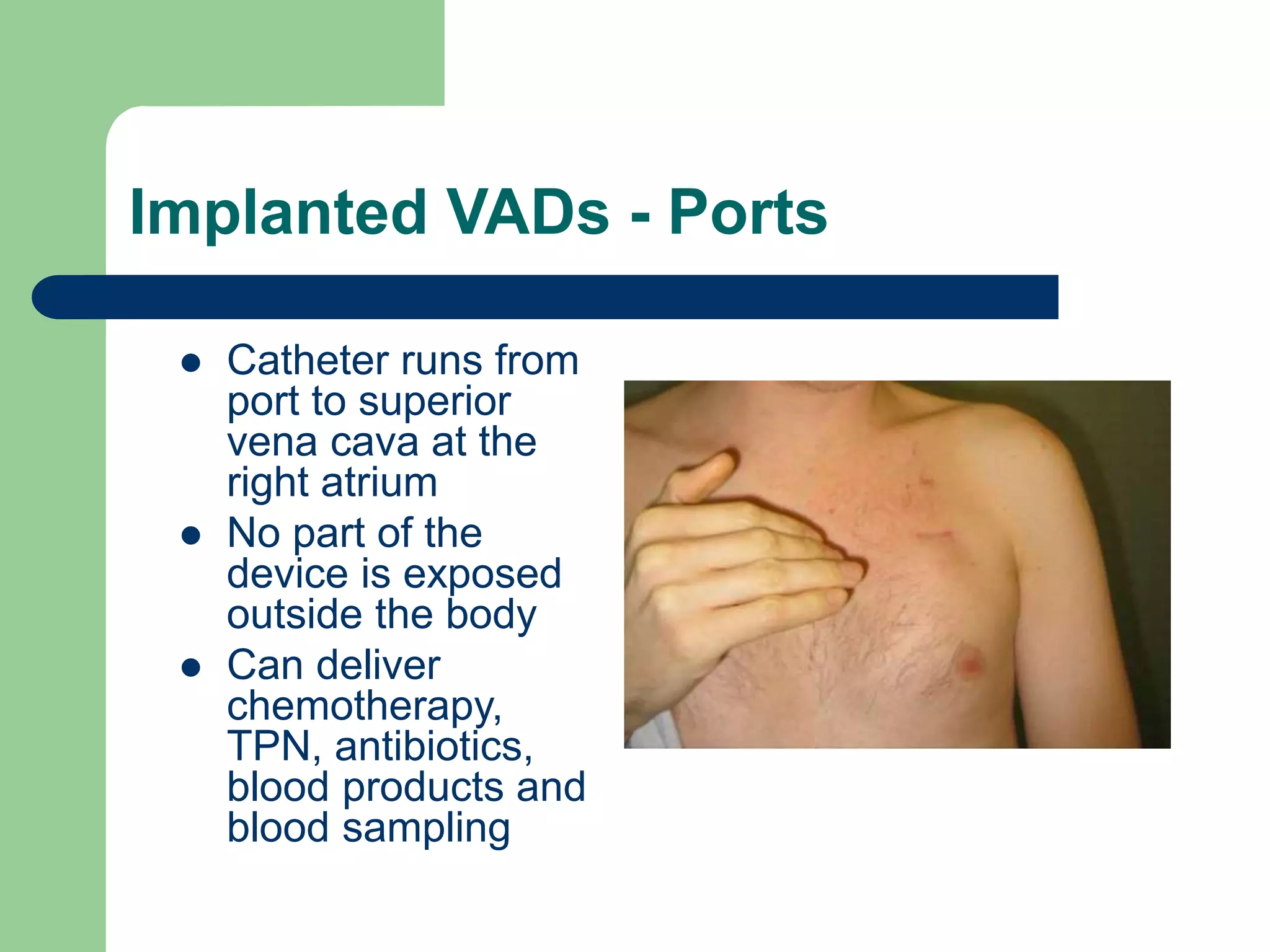
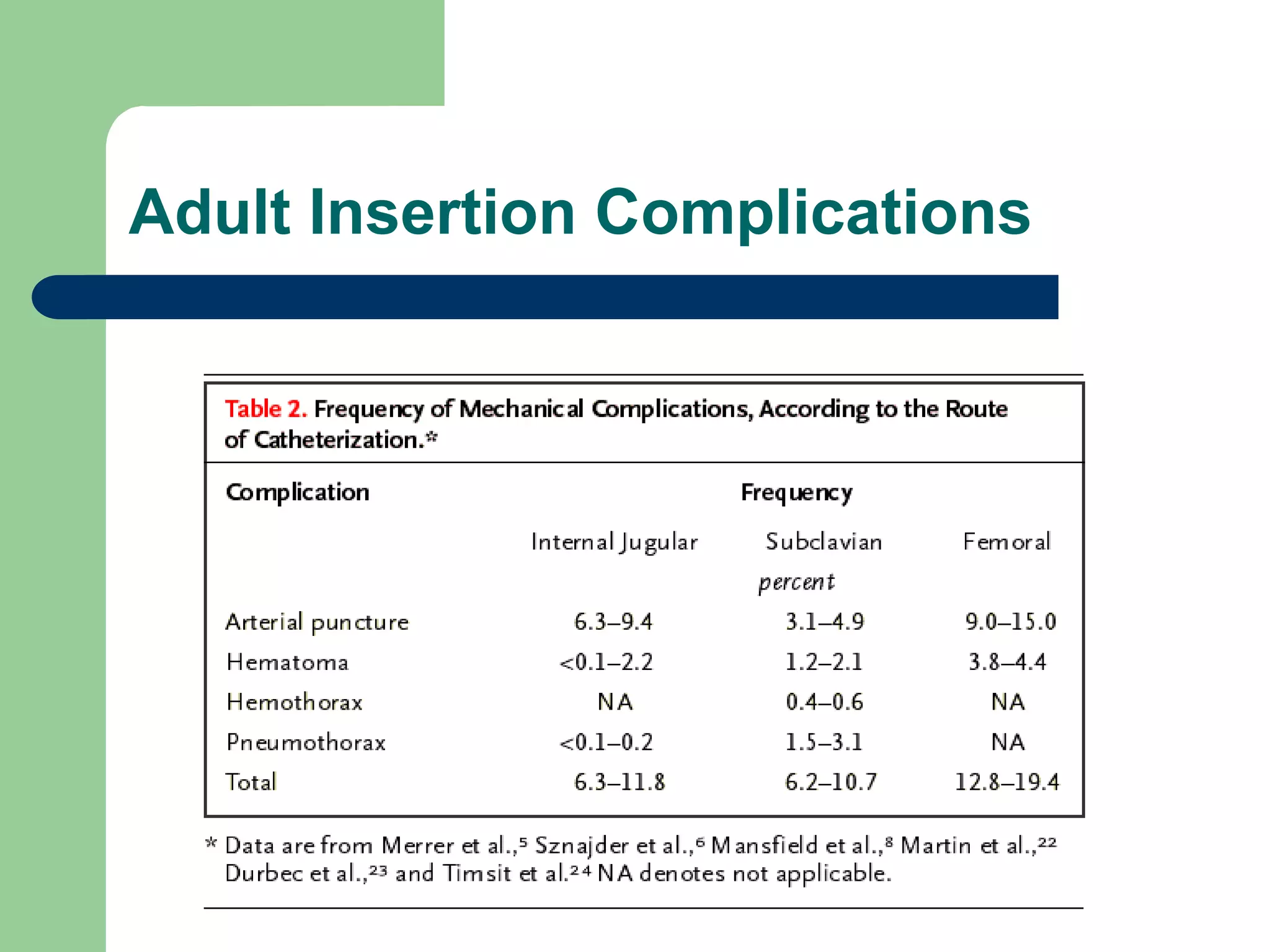
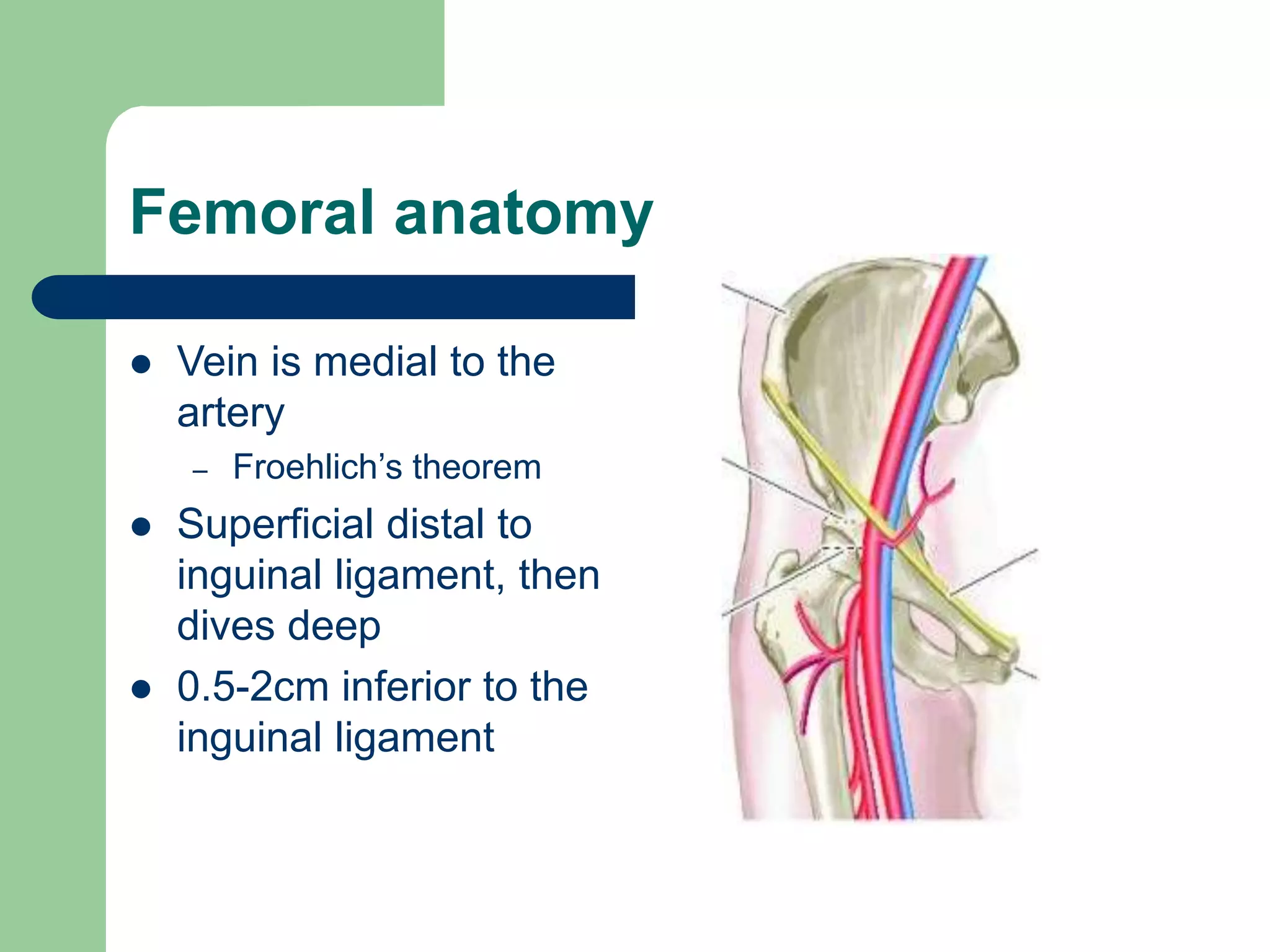
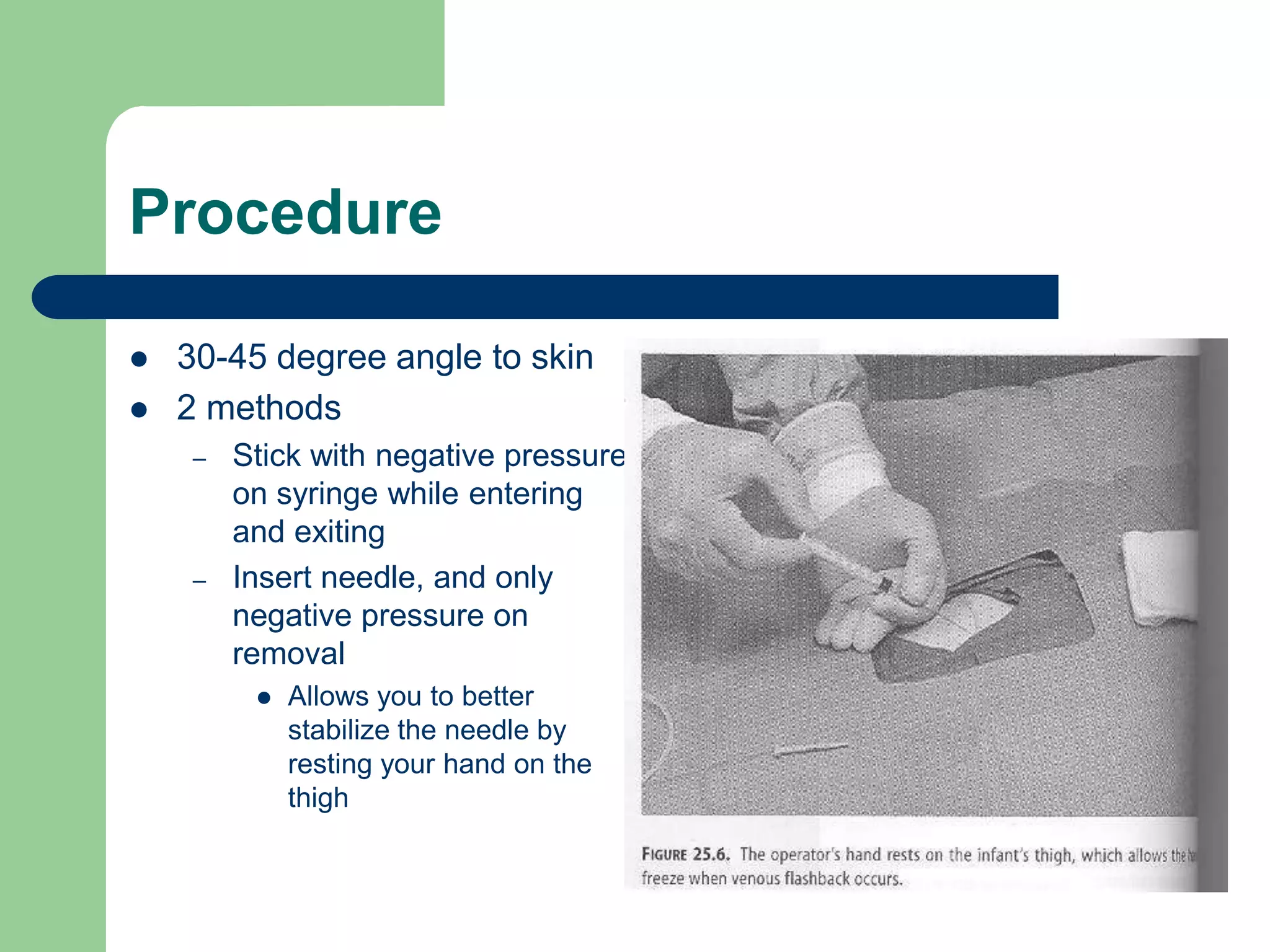
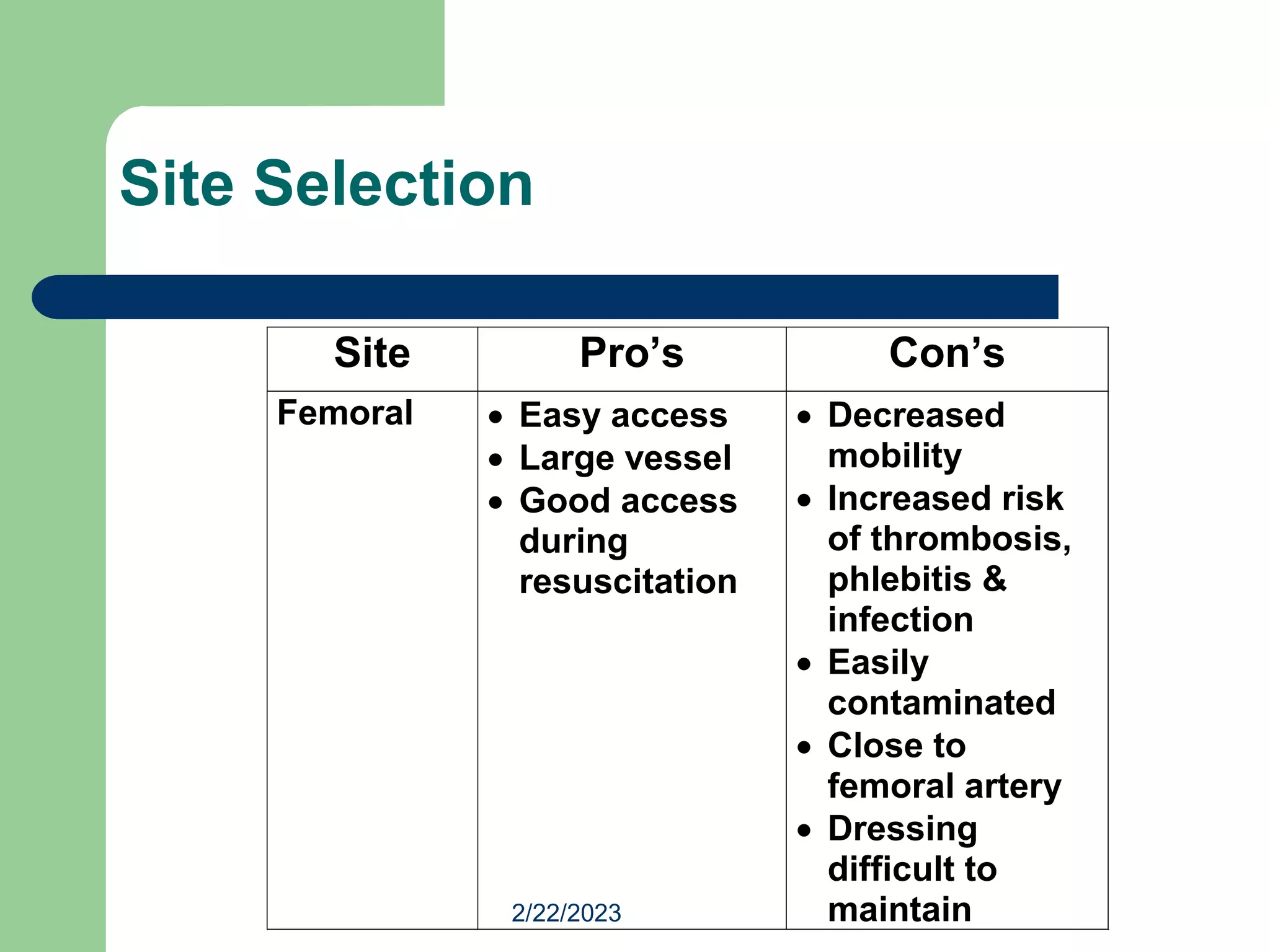
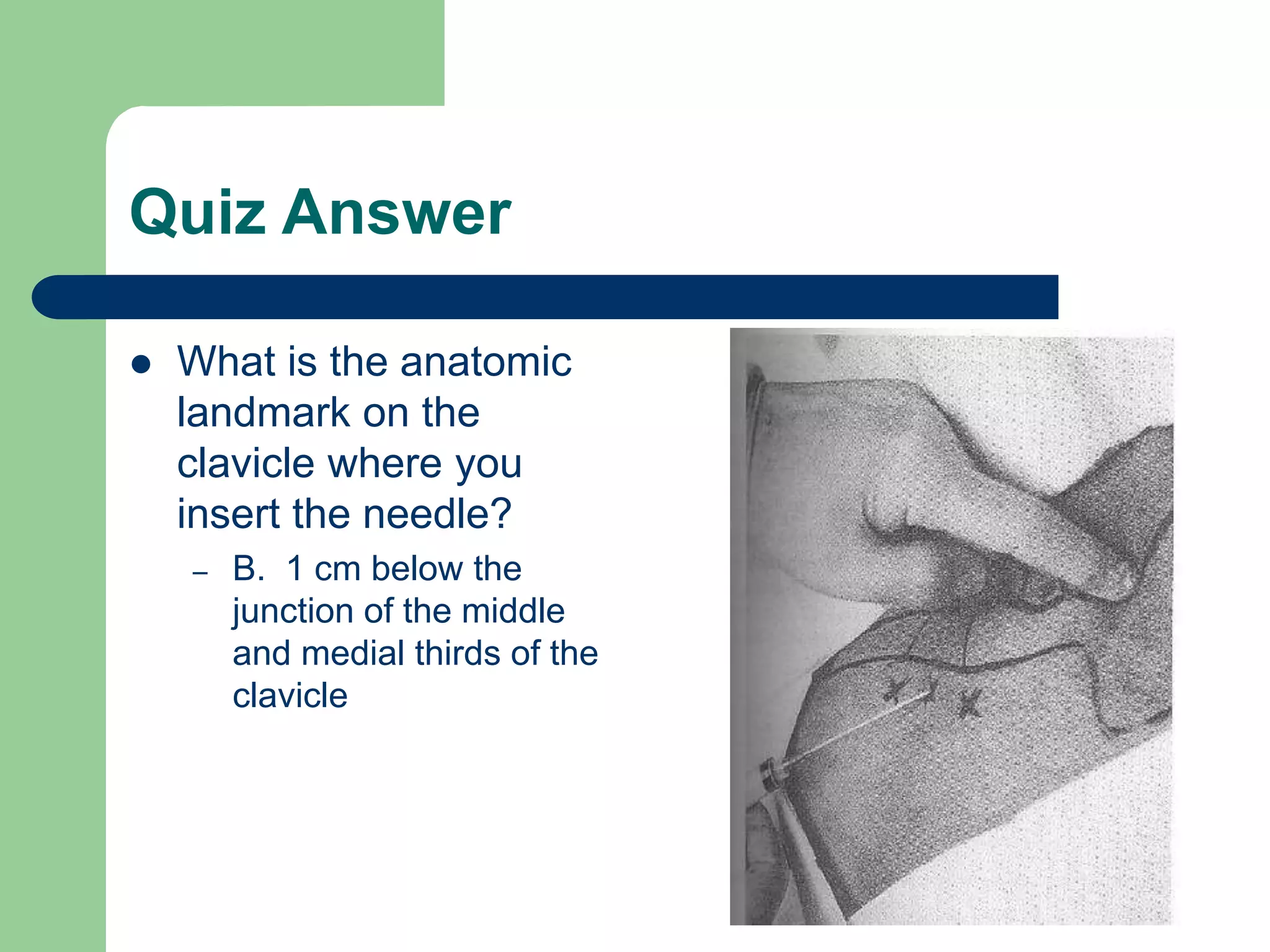
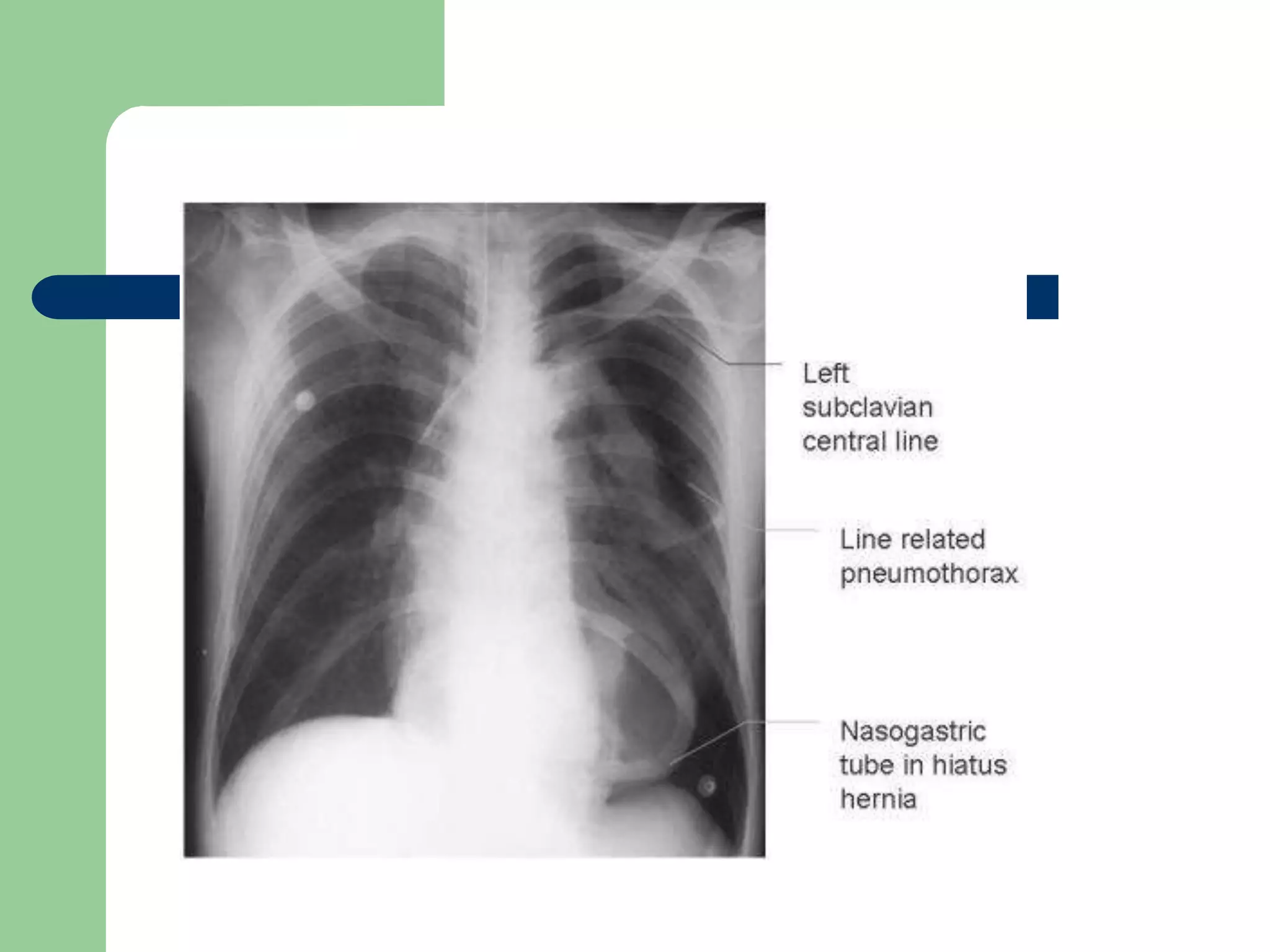
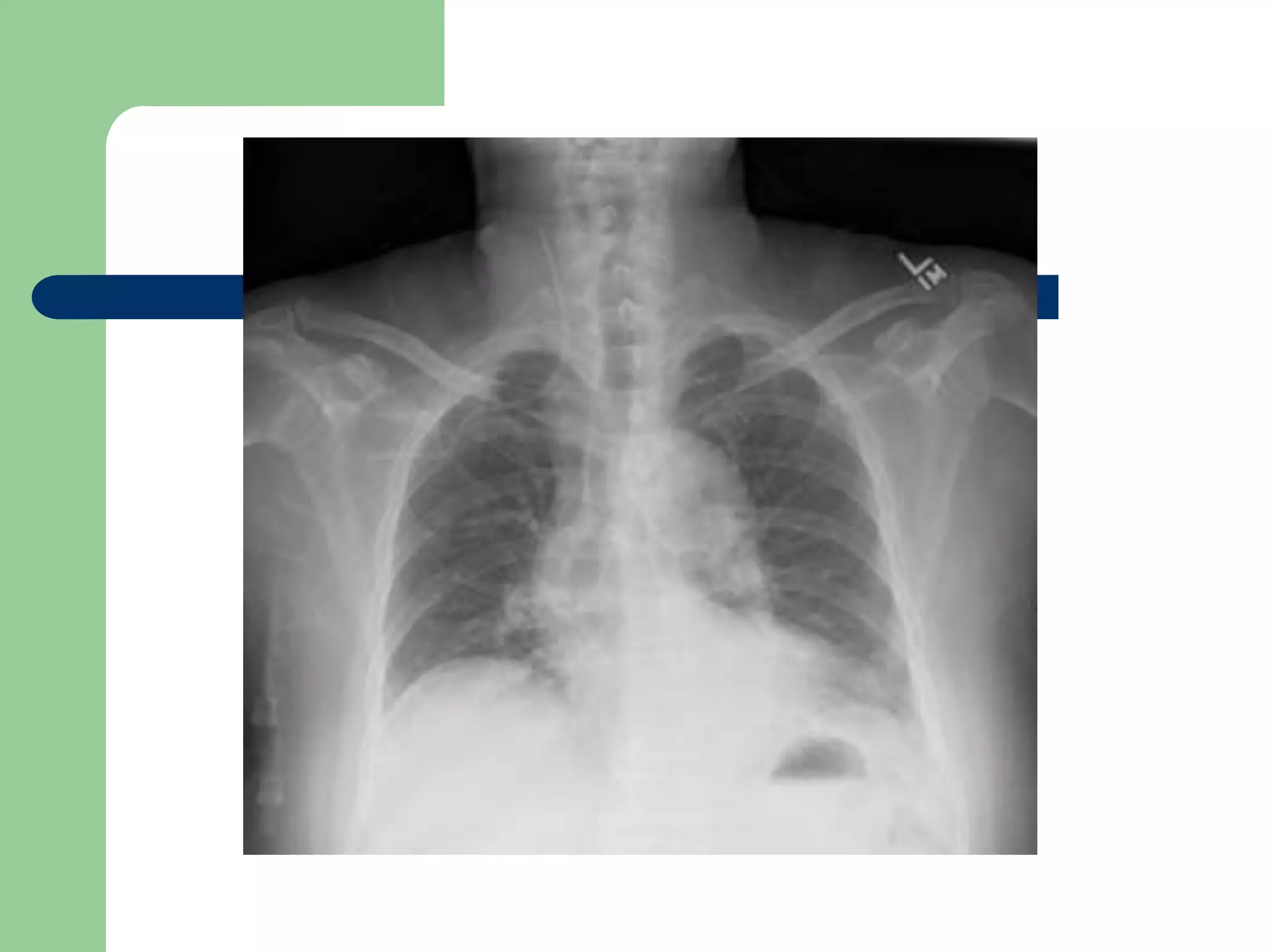
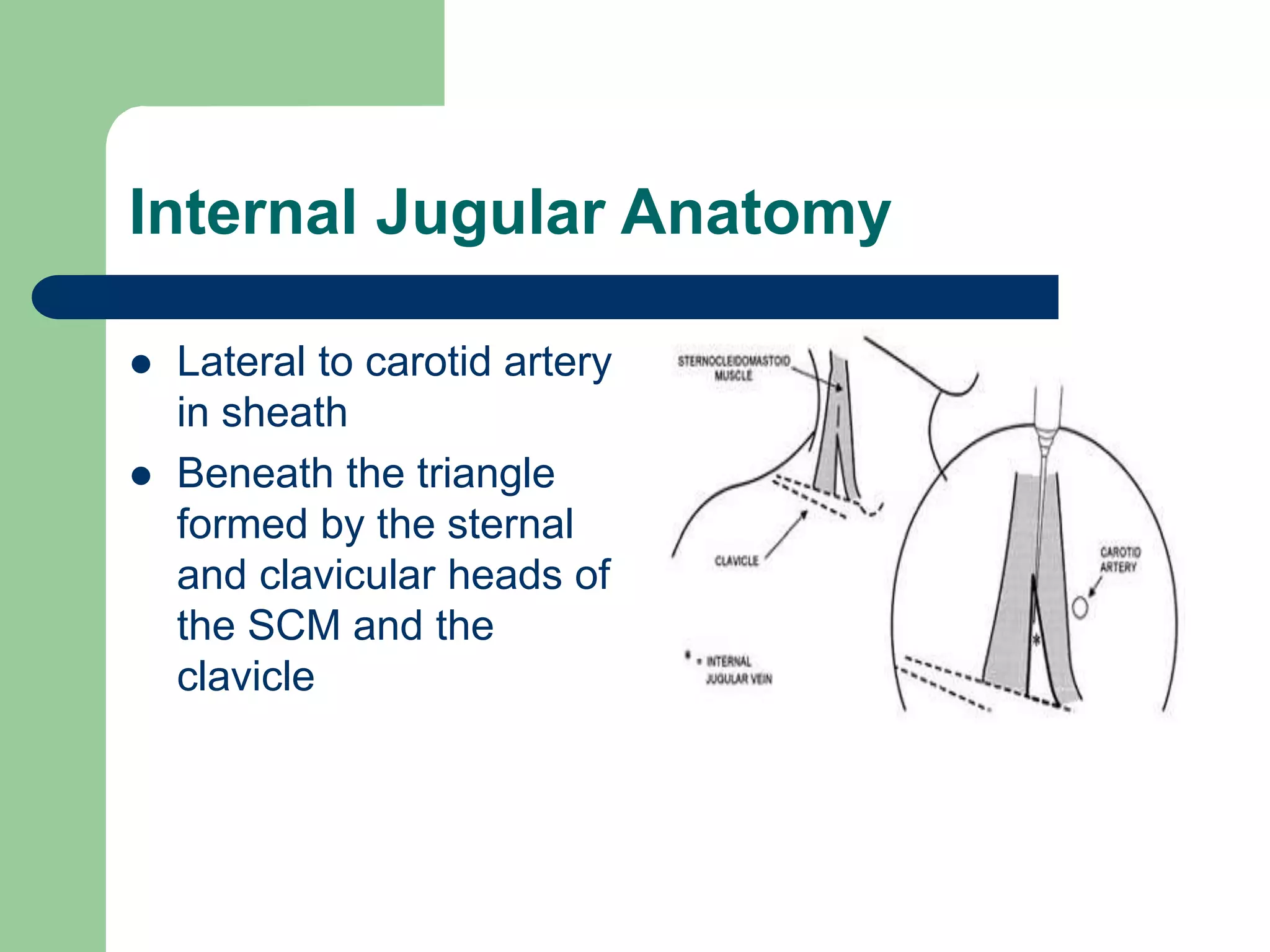
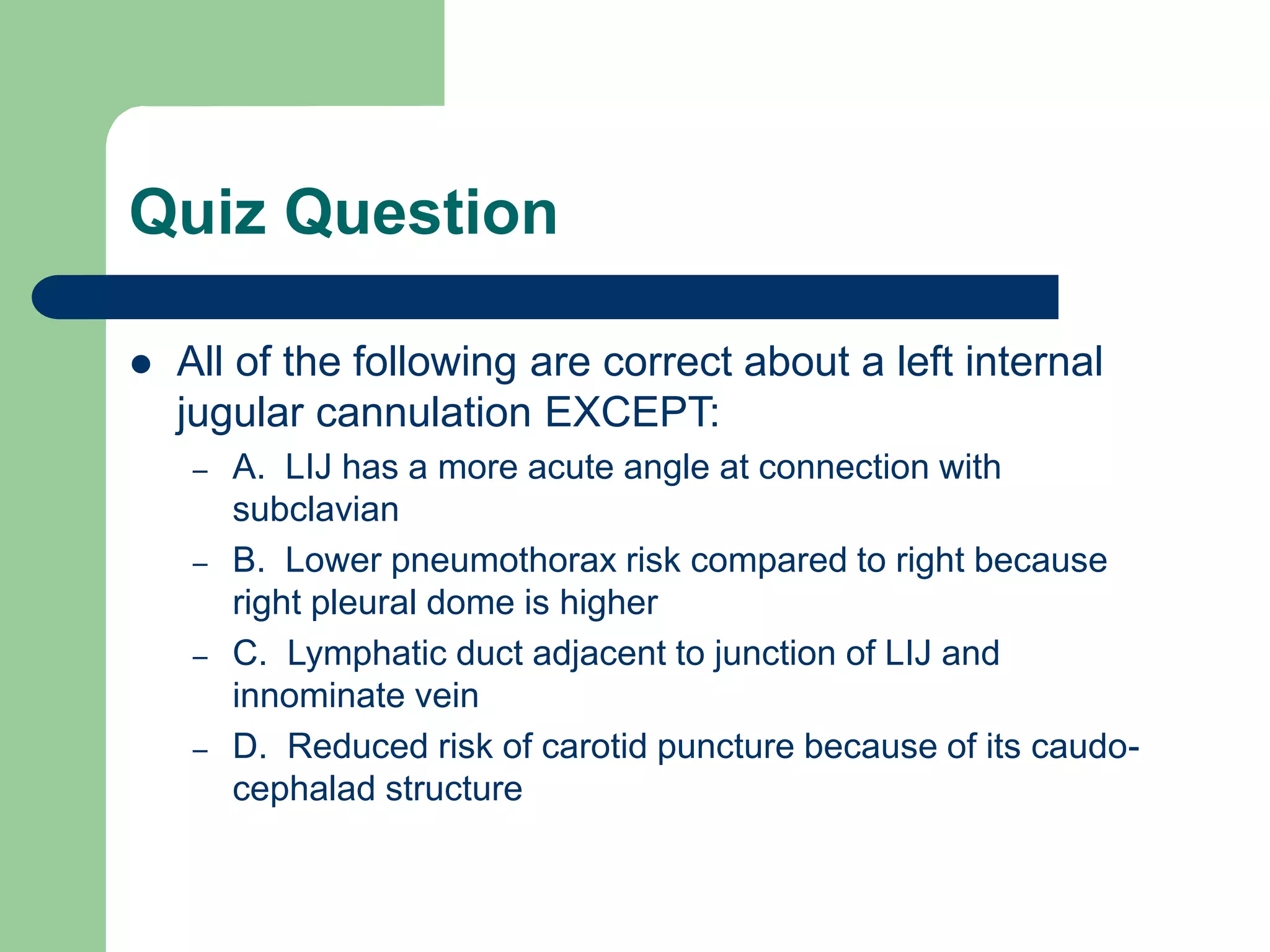
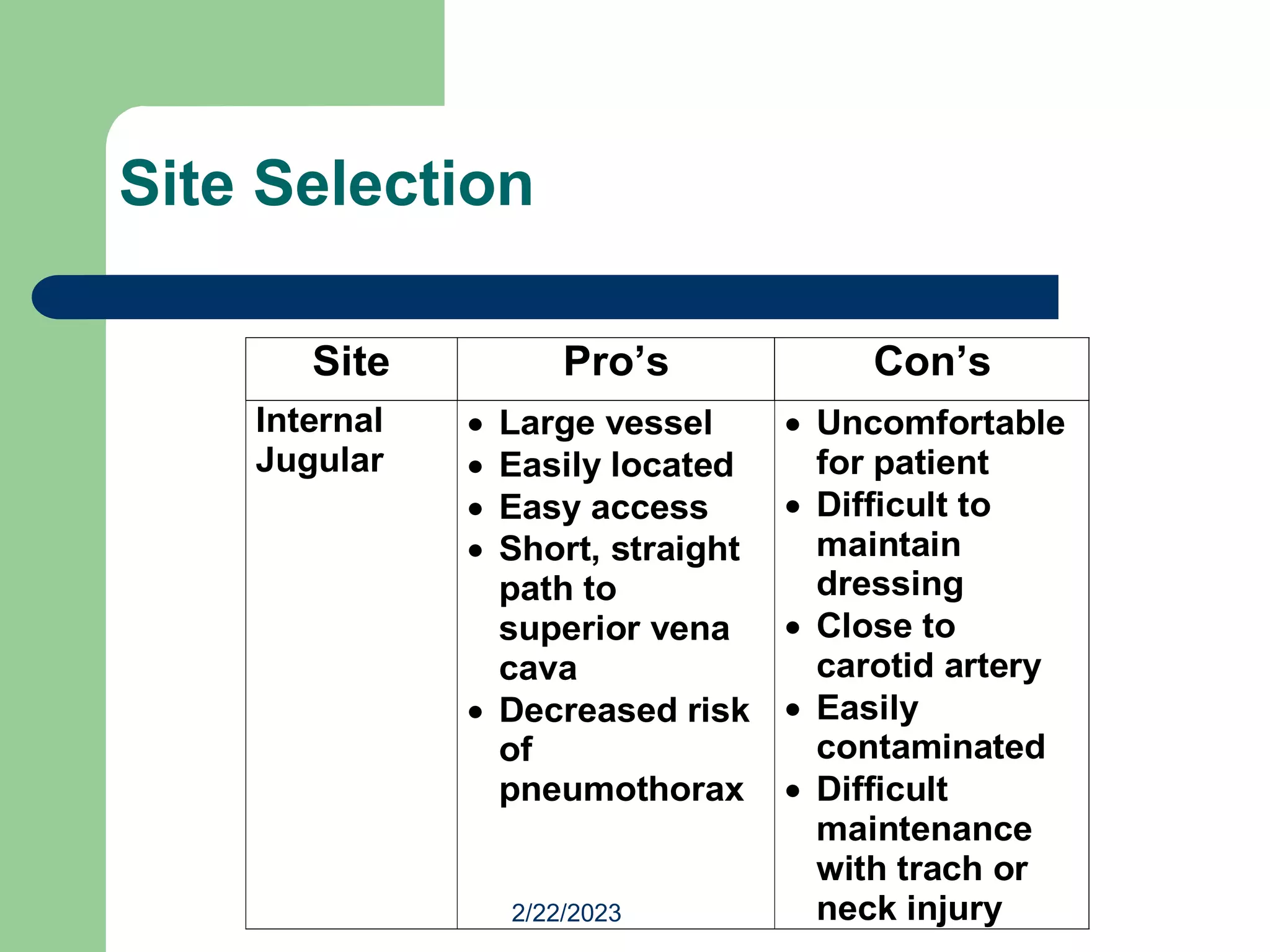
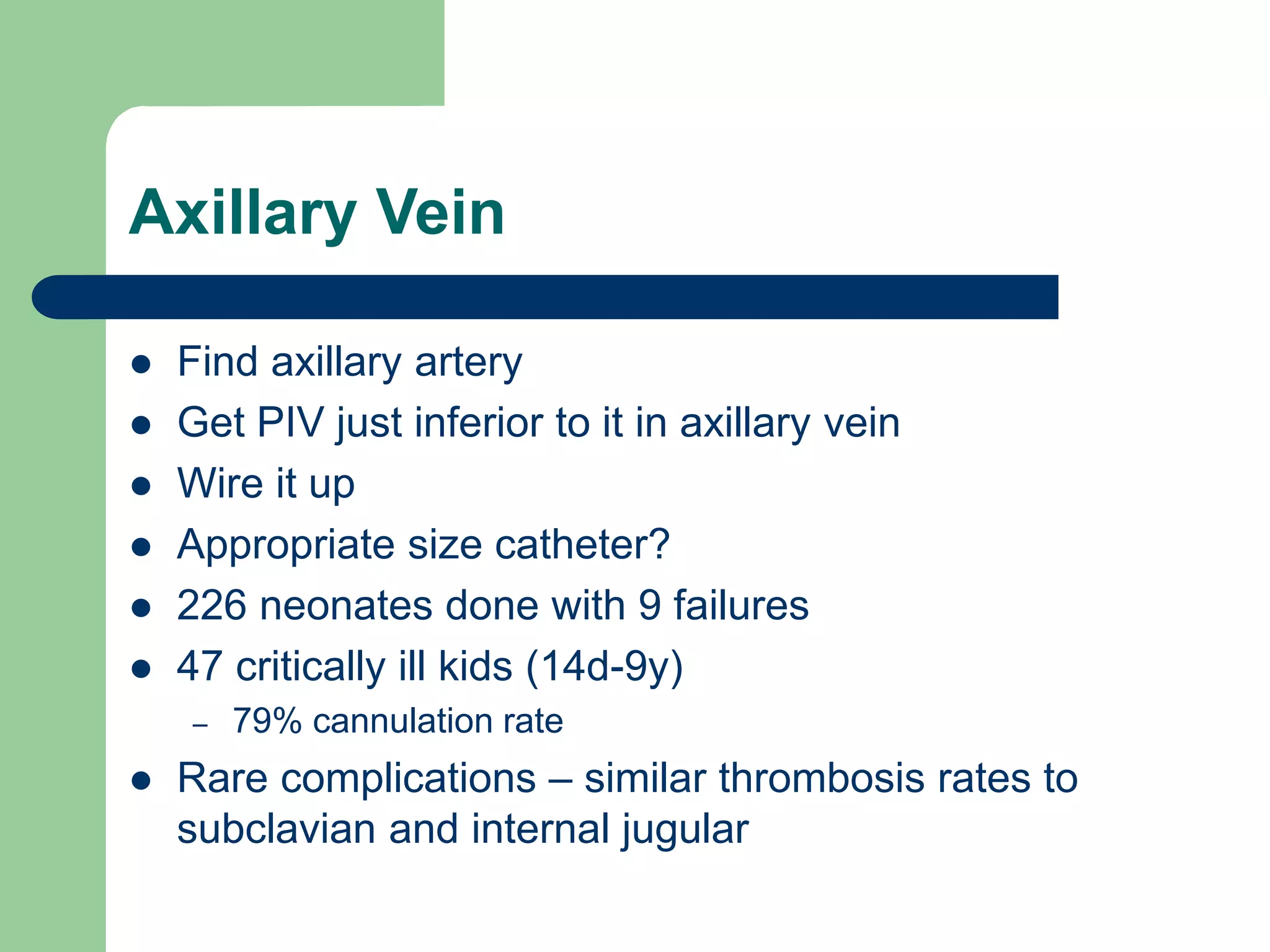
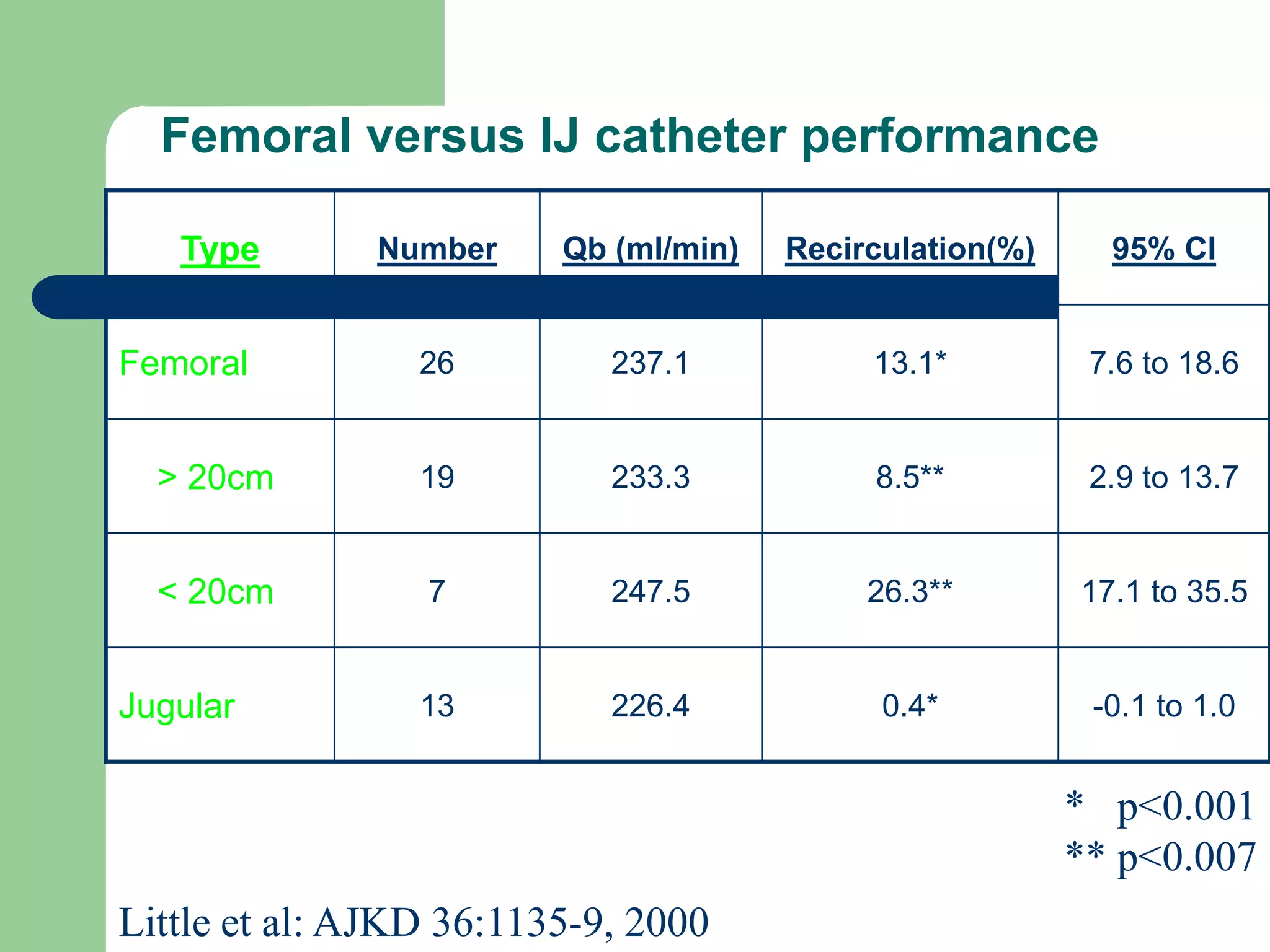
This document discusses various types of venous access in children, including peripheral IVs, peripherally inserted central catheters (PICCs), midlines, central venous catheters (CVCs), tunneled catheters, and implanted ports. It provides details on insertion sites such as the forearm, hand, femoral, subclavian, and internal jugular veins. Complications of placement like infiltration, extravasation, and infection are also reviewed. The document emphasizes using the safest and most distal sites first when placing peripheral IVs and discusses techniques and landmarks for central line placement.