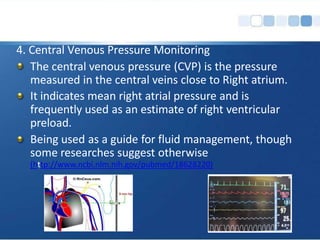
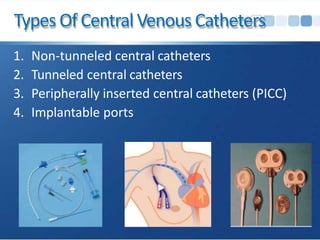
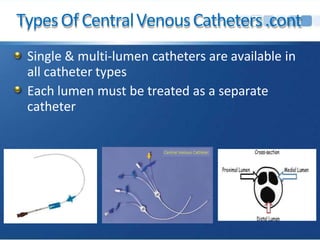
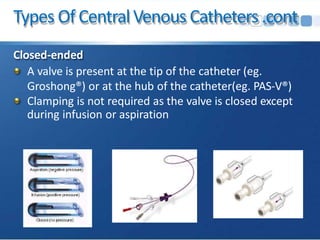
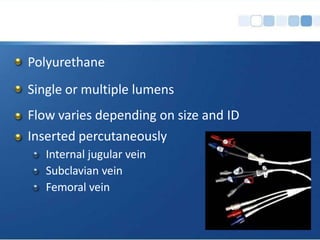
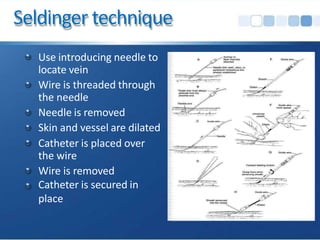
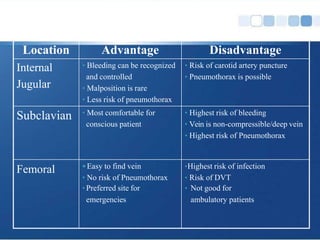
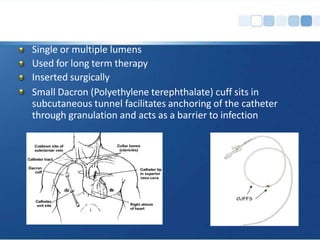
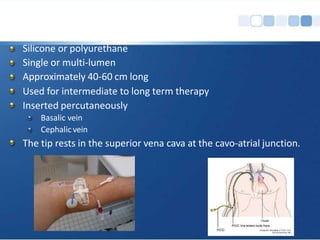
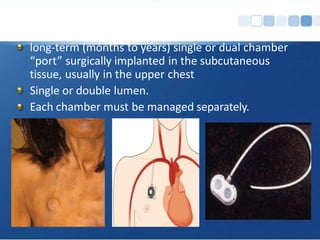
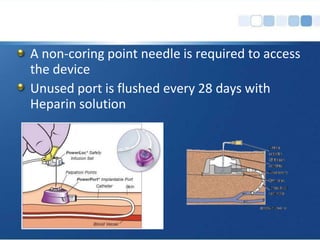
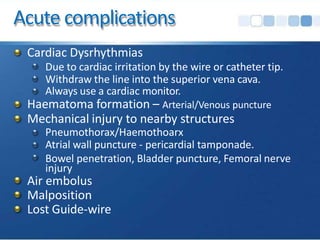
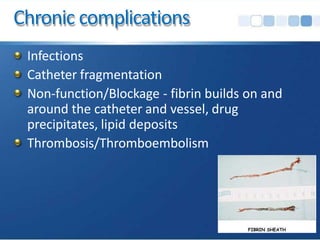
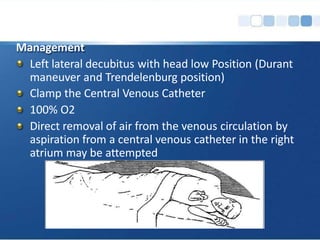
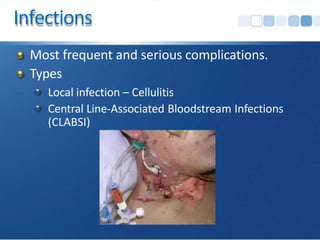
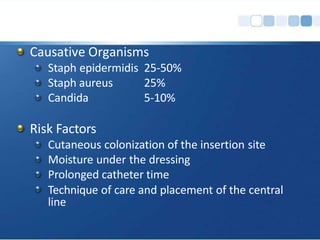
This document discusses central venous catheters and their uses, types, insertion techniques, complications, and strategies to reduce infections. Central venous catheters are indwelling intravenous devices inserted into central veins for difficult vascular access, volume loading of medications or solutions, central venous pressure monitoring, and hemodialysis. Types include non-tunneled, tunneled, peripherally inserted central catheters, and implantable ports. Complications can be acute like hematoma or pneumothorax, or chronic like infections, thrombosis, and non-function. Infection is the most serious complication and strategies like hand hygiene and chlorhexidine skin preparation can reduce central line-associated bloodstream infections.