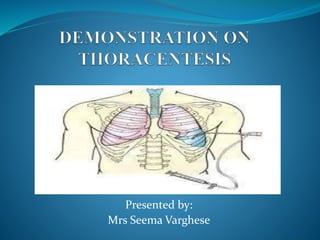
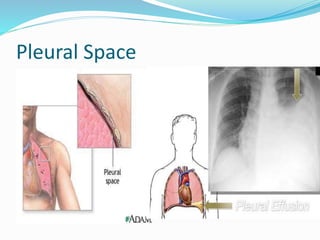
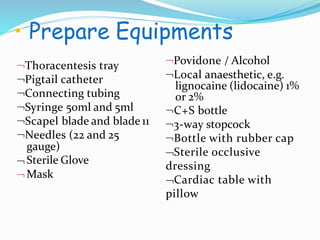
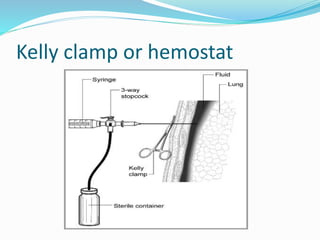
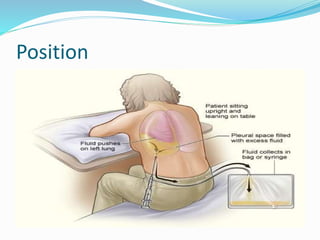
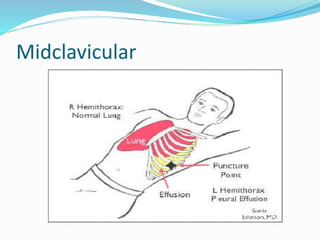
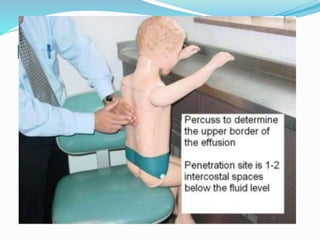
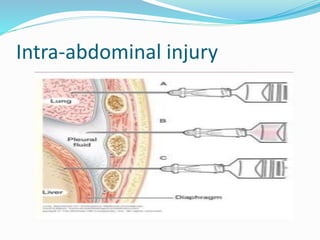
Thoracentesis is a procedure to drain fluid from the pleural space around the lungs. It involves inserting a large bore needle through the chest wall under local anesthesia. The fluid is drained to diagnose the cause of excess fluid or provide relief from symptoms. Nurses prepare equipment, position the patient, monitor them during the procedure, and assess for complications like pneumothorax afterwards. Proper documentation and care of any insertion site is also important. Thoracentesis can help determine the cause of pleural effusions and relieve symptoms like shortness of breath.