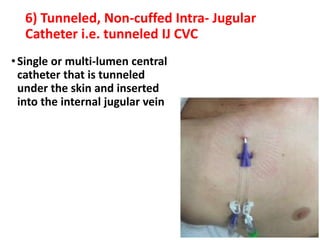
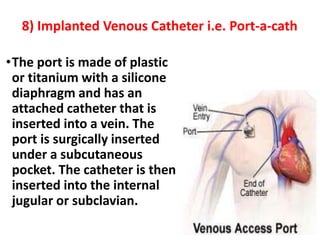
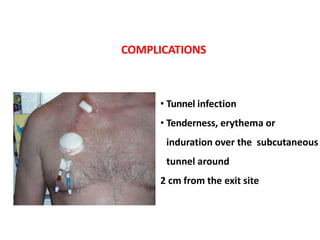
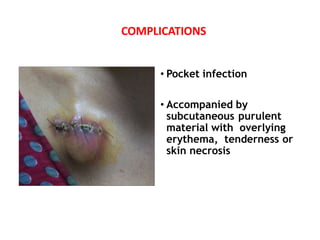
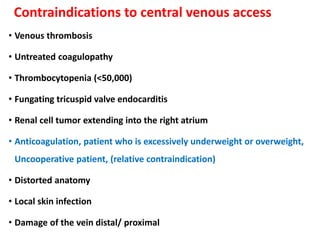
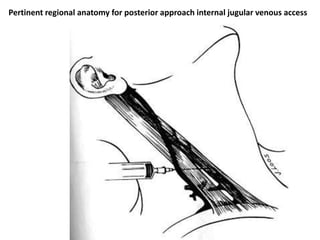
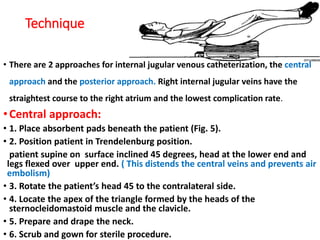
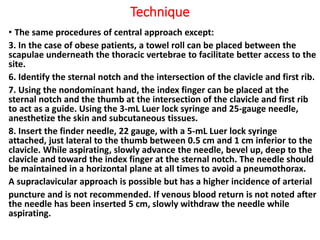
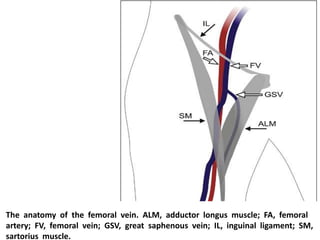
A central venous catheter (central line) is a large vein catheter used for medication administration and medical monitoring, often placed in the internal jugular, subclavian, or femoral veins. The procedure carries risks such as infection and thrombosis, with specific indications and contraindications for use based on patient condition. Proper technique and post-placement care are essential to minimize complications and ensure patient safety.






























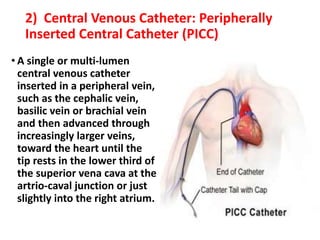
![Peripherally inserted central catheters[PICC]](https://image.slidesharecdn.com/centralline-220909144158-5bad2fd3/85/central-line-pptx-41-320.jpg)