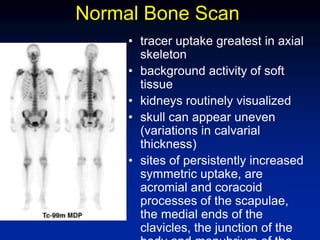
Bone scintigraphy uses radiolabeled phosphonates injected intravenously to evaluate bone formation. It produces whole body images of tracer distribution in the skeleton. Increased uptake indicates elevated osteoblastic activity such as might occur with fractures, tumors, or metastases. The scan has high sensitivity but low specificity for bone abnormalities, so findings must be interpreted in clinical context. It is useful for detecting skeletal involvement by cancer or other bone diseases.

![• Technetium-99m medronate (methylene
diphosphonate [MDP]),
• technetium-99m oxidronate
(hydroxymethylene diphosphonate
[HMDP]),
• or hydroxyethylene diphosphonate (HDP)
is administered intravenously.](https://image.slidesharecdn.com/bonescanning-140313053917-phpapp02/85/Bone-scan-13-320.jpg)





![• The first (dynamic) phase reflects the
relative amount of blood flow to the
area of interest, whereas the second
(blood pool) phase reflects the amount
of activity that has extravasated into
the tissues around the area of interest.
The third (delayed [bone]) phase
reflects the rate of bone turnover.
• The classic appearance of
osteomyelitis on three-phase bone
scans consists of focal hyperperfusion,
focal hyperemia, and focally increased](https://image.slidesharecdn.com/bonescanning-140313053917-phpapp02/85/Bone-scan-60-320.jpg)