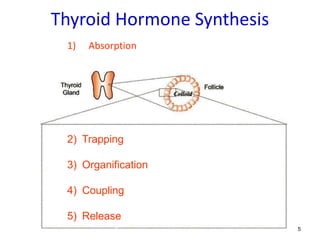
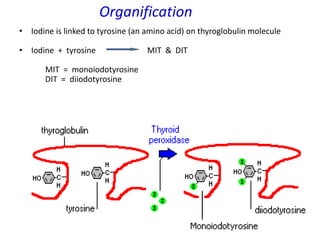
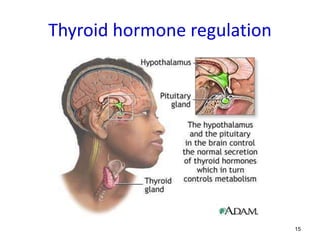
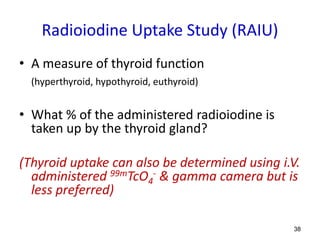
The thyroid gland sits in front of the trachea. It synthesizes the hormones T3 and T4 through a process involving absorption of iodine from the diet, trapping of iodide in thyroid follicular cells, organification of iodide by binding it to tyrosine residues on thyroglobulin, coupling of iodotyrosines to form the hormones, and release of T3 and T4 into circulation in response to TSH. Thyroid imaging using radiopharmaceuticals like Tc-99m pertechnetate, I-123, or I-131 allows evaluation of thyroid anatomy and function through visualization and quantification of radiotracer uptake.