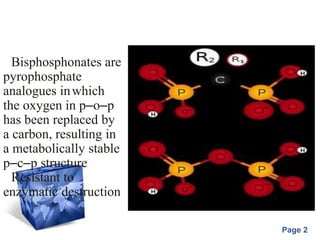
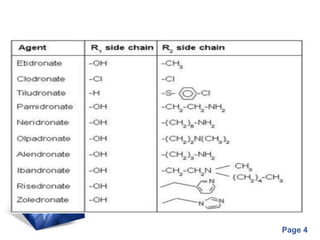
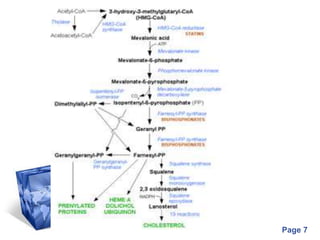
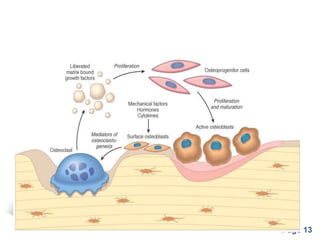
Bisphosphonates are pyrophosphate analogues that are resistant to enzymatic destruction and bind strongly to bone. They are used to treat osteoporosis, Paget's disease, and bone metastases. Newer generations of bisphosphonates are more potent and selectively inhibit bone resorption over formation. They work by inhibiting enzymes in the HMG-CoA reductase pathway, preventing osteoclast function. Clinical trials demonstrate bisphosphonates' ability to increase bone mineral density and reduce fracture risk. While generally well-tolerated, they can cause jaw necrosis or atypical femoral fractures with prolonged use.