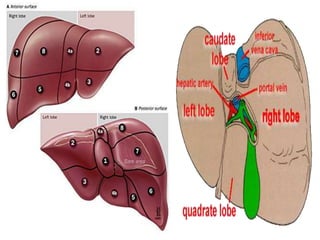
1. Liver lies in right hypochondrium and divided in to right and left lobes.
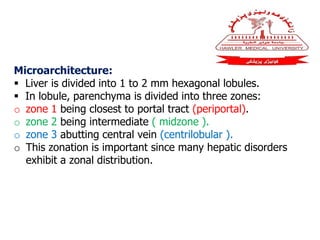
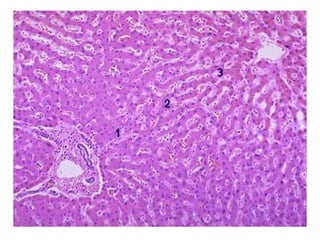
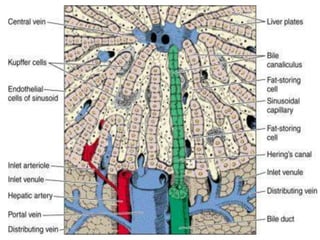
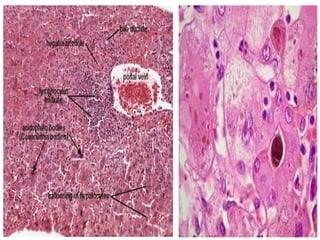
2. Microarchitecture : liver is divided into 1 to 2 mm hexagonal lobules.
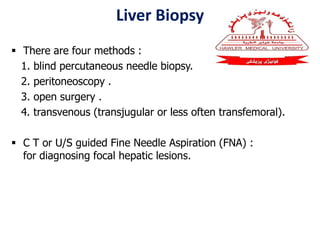
3. There are four methods for liver biopsy.
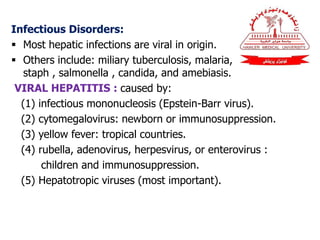
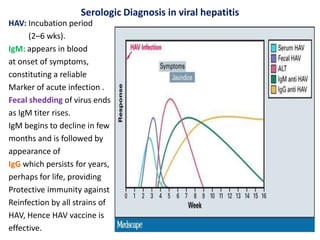
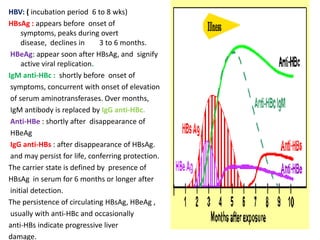
4. Most hepatic infections are viral in origin.
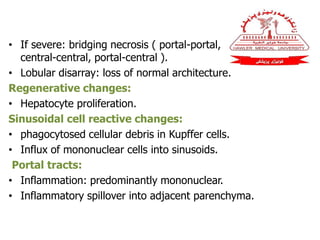
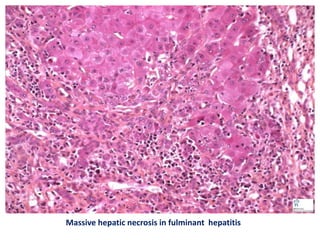
5. In fulminant hepatitis hepatic insufficiency progresses from onset of symptoms to hepatic encephalopathy within2 to 3 weeks.