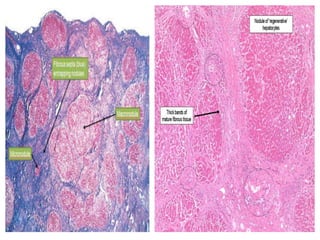
1. Liver cirrhosis is the end stage of many chronic liver diseases and is characterized by diffuse hepatic fibrosis and parenchymal nodule formation.
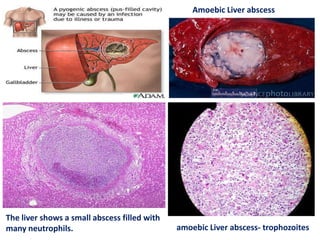
2. Liver abscesses can be caused by parasitic or pyogenic infections and present as solitary or multiple lesions on gross and microscopic examination.
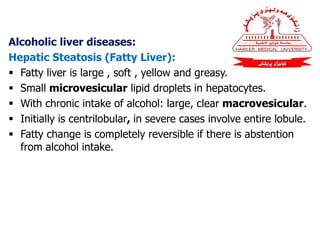
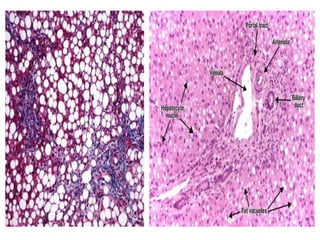
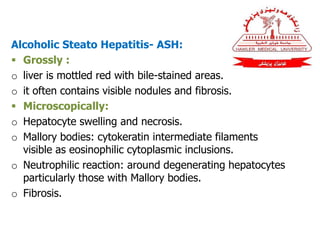
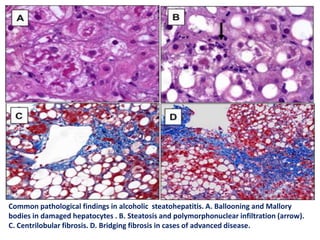
3. Alcoholic liver diseases include fatty liver, alcoholic steatohepatitis (ASH), and alcoholic cirrhosis, progressing from steatosis to necroinflammation and fibrosis.