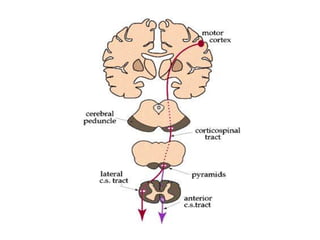
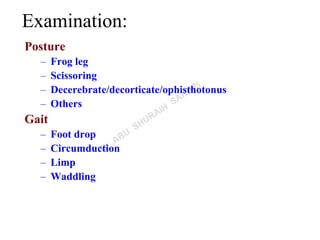
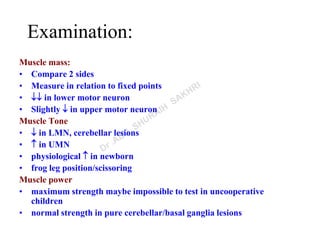
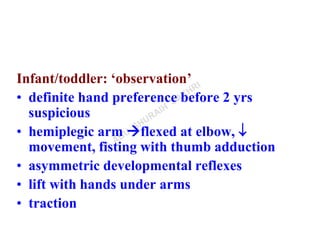
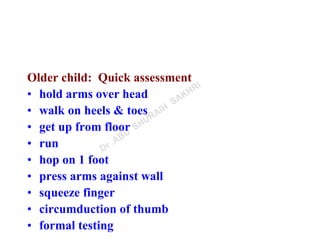
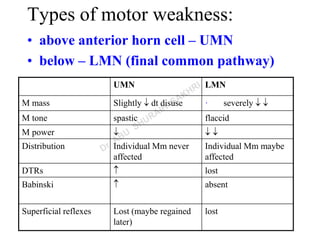
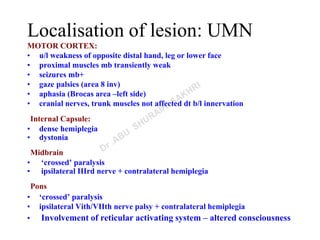
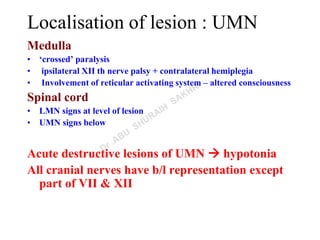
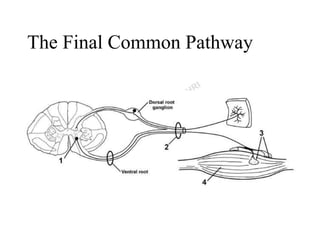
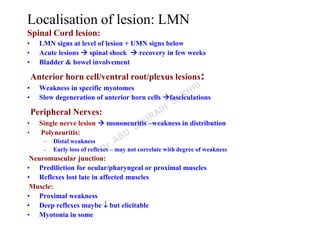
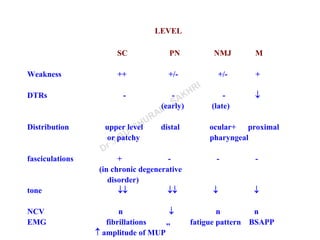
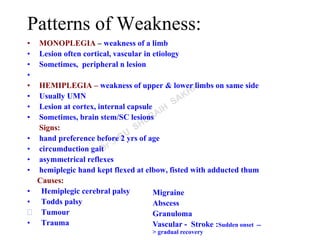
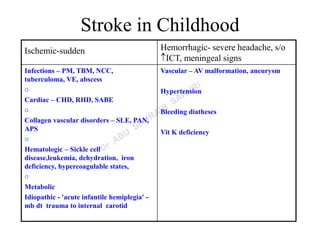
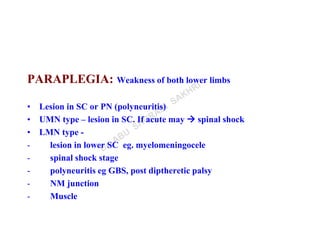
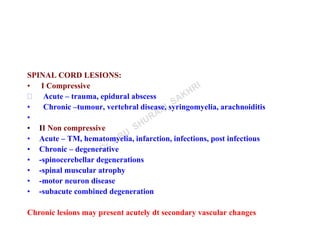
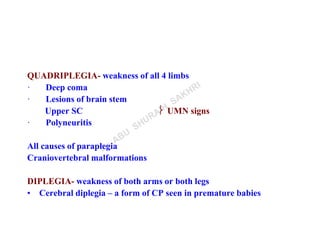
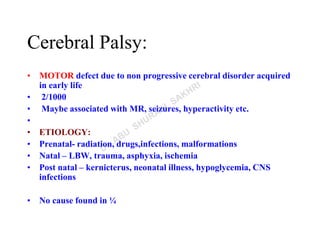
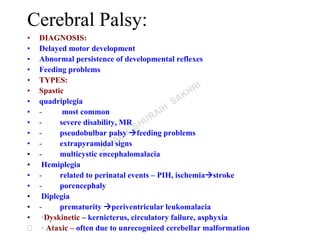
This document discusses motor weakness, including the types, patterns, localization of lesions, and examination. It describes upper motor neuron and lower motor neuron weakness, and patterns such as monoplegia, hemiplegia, paraplegia, quadriplegia, and diplegia. The document provides details on examining posture, gait, muscle mass, tone, power, coordination and reflexes. It also discusses localizing lesions to different areas of the brain or spinal cord based on the clinical signs. Cerebral palsy is discussed as a common cause of motor weakness in children.