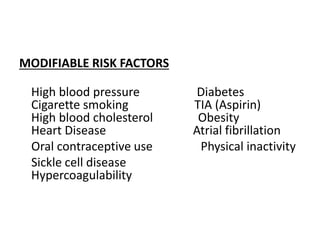
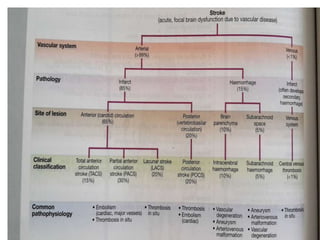
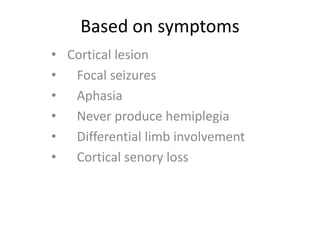
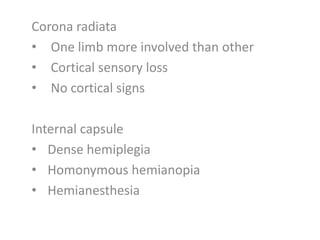
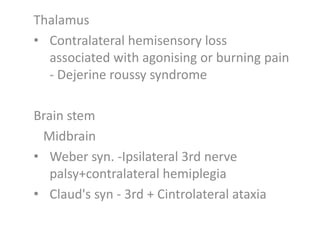
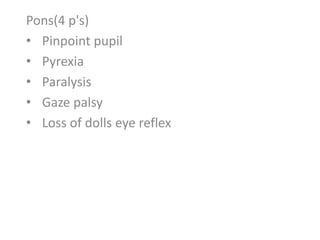
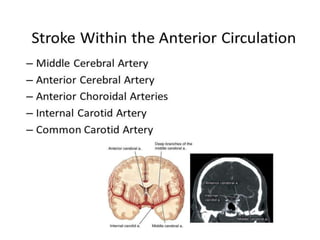
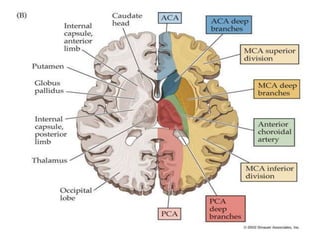
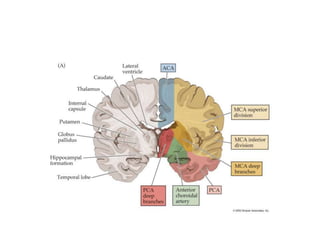
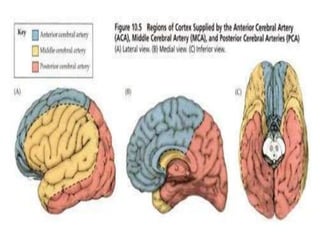
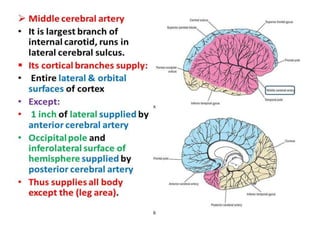
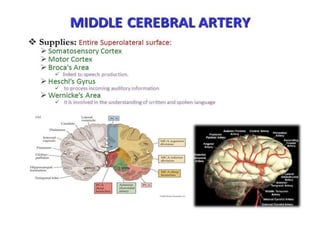
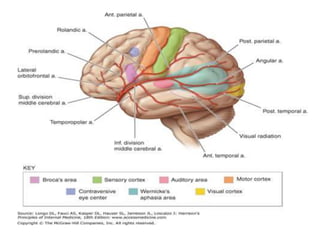
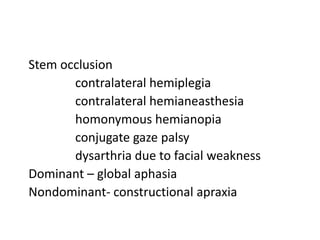
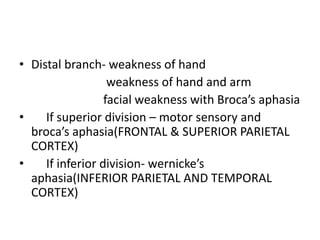
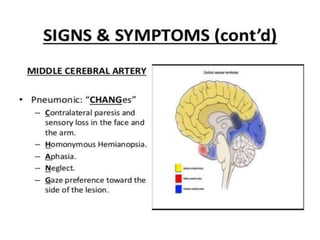
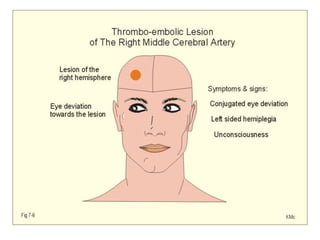
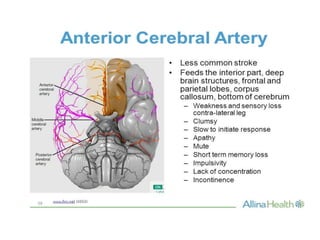
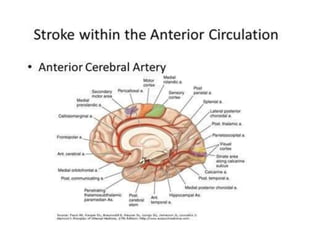
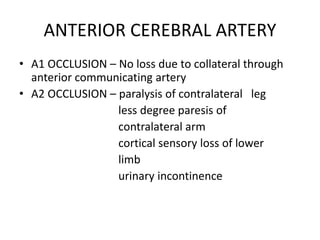
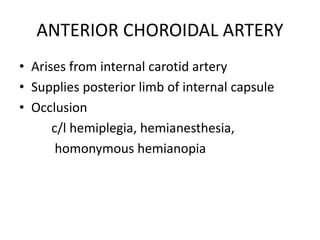
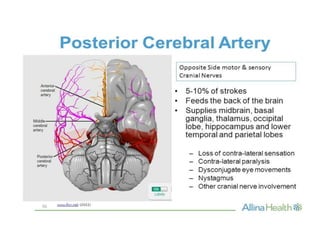
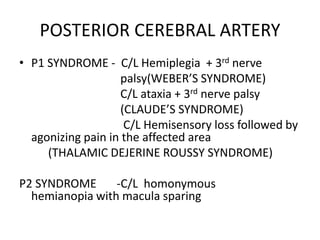
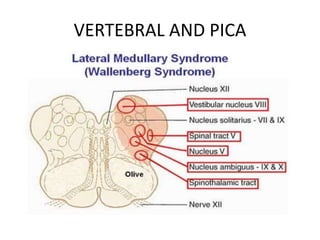
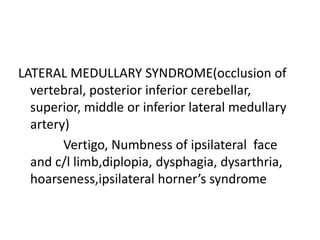
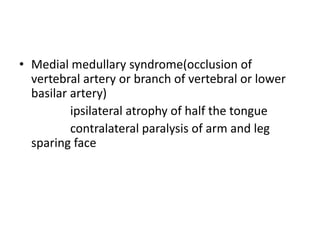
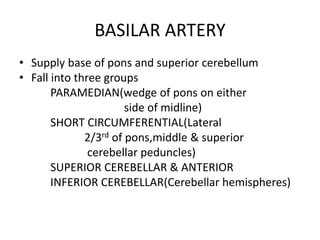
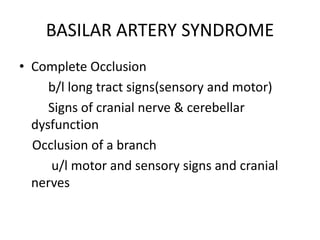
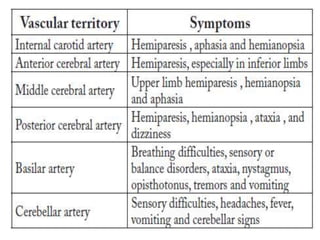
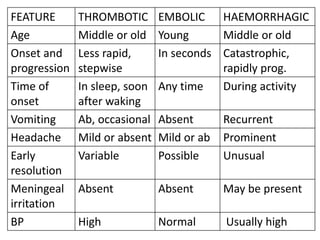
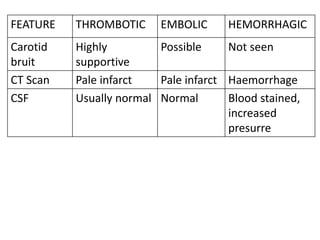
This document discusses the localization, risk factors, and clinical presentations of different types of strokes. It describes that strokes are caused by focal vascular issues that last more than 24 hours. Risk factors include non-modifiable factors like age and heredity, as well as modifiable factors like high blood pressure, diabetes, smoking, and atrial fibrillation. Different vascular territories are associated with specific neurological deficits, such as the middle cerebral artery with hemiplegia and sensory loss. Various artery occlusions, including the anterior and posterior cerebral arteries, can cause deficits based on their vascular supply regions.