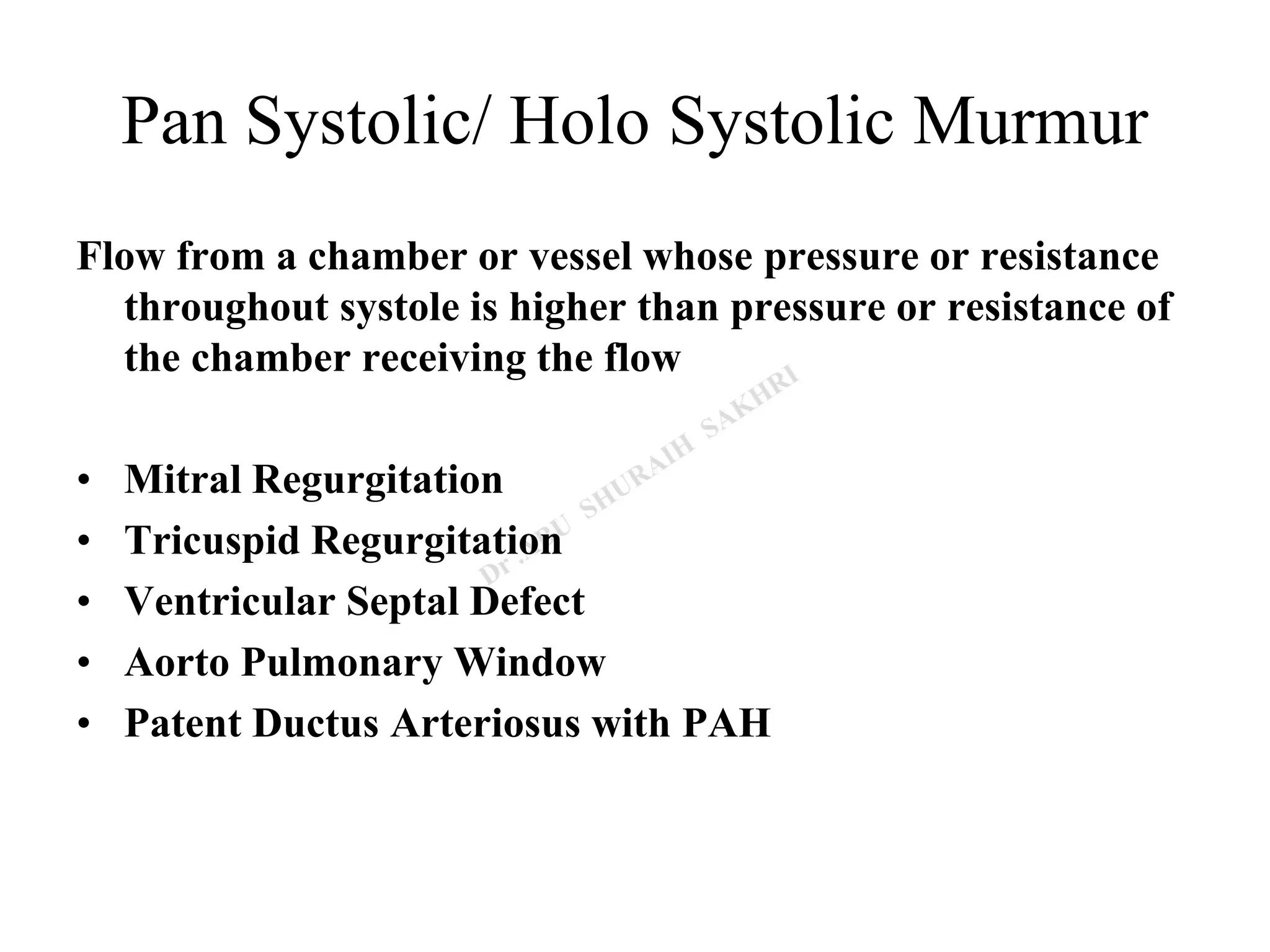
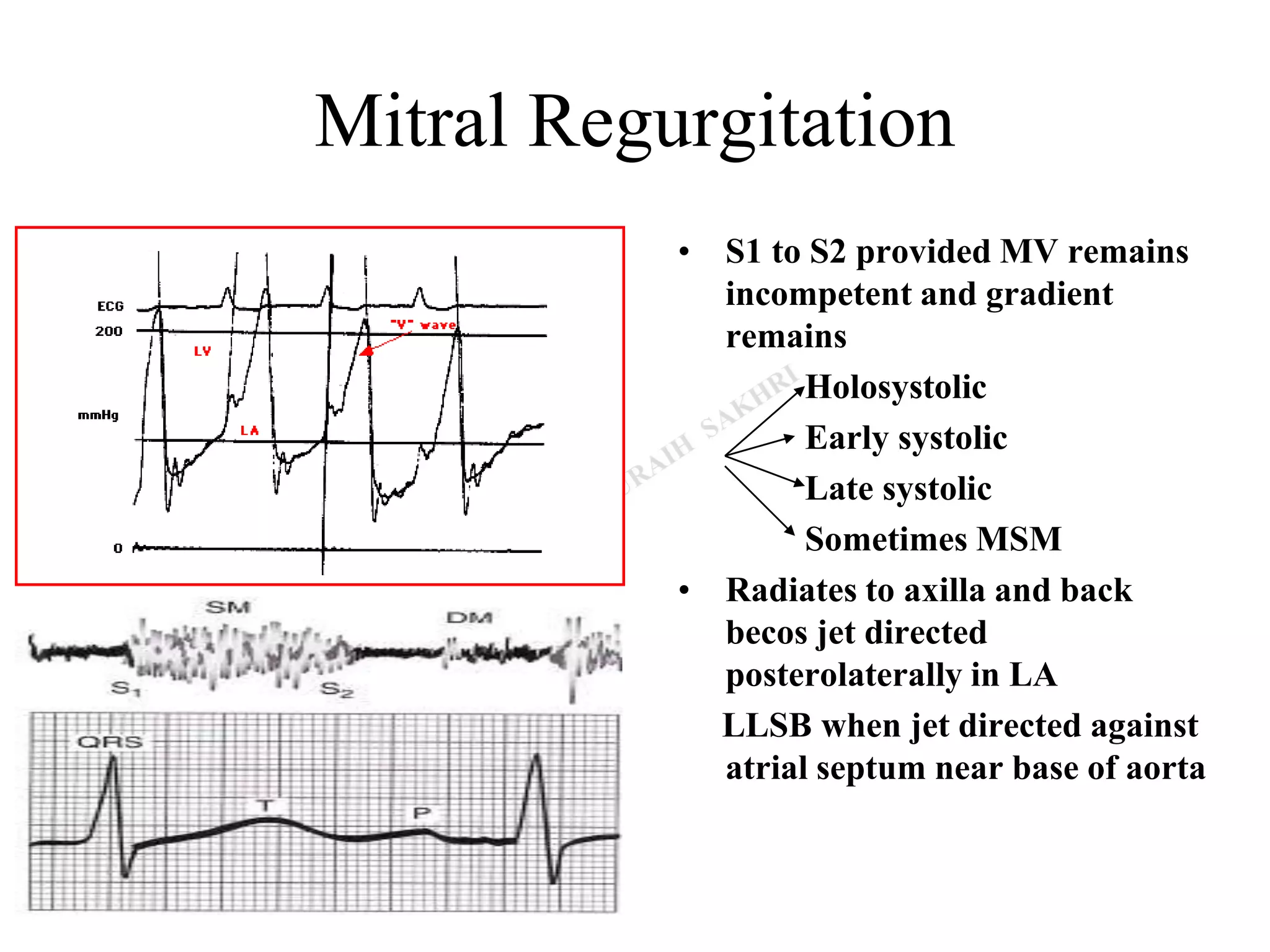
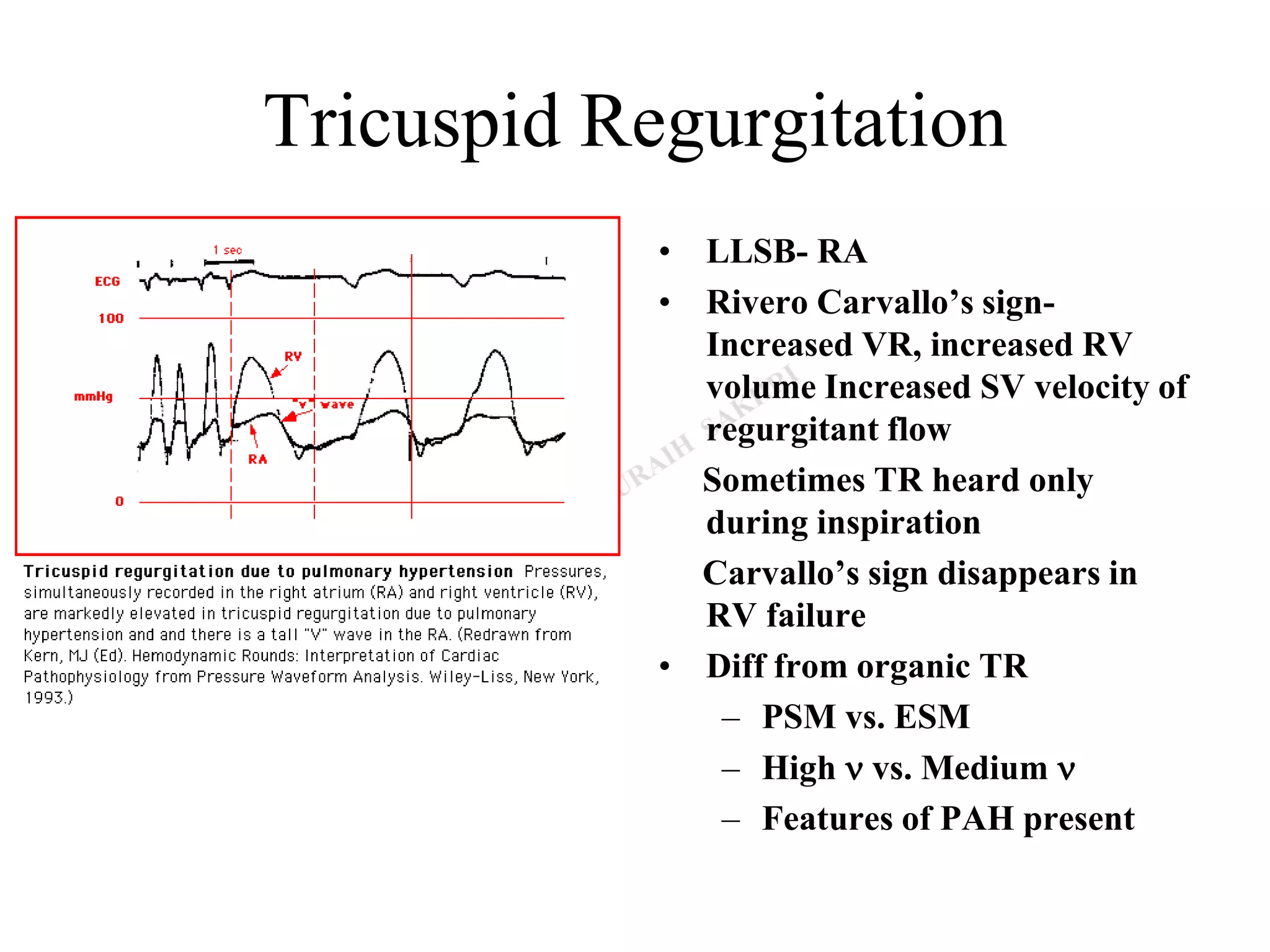
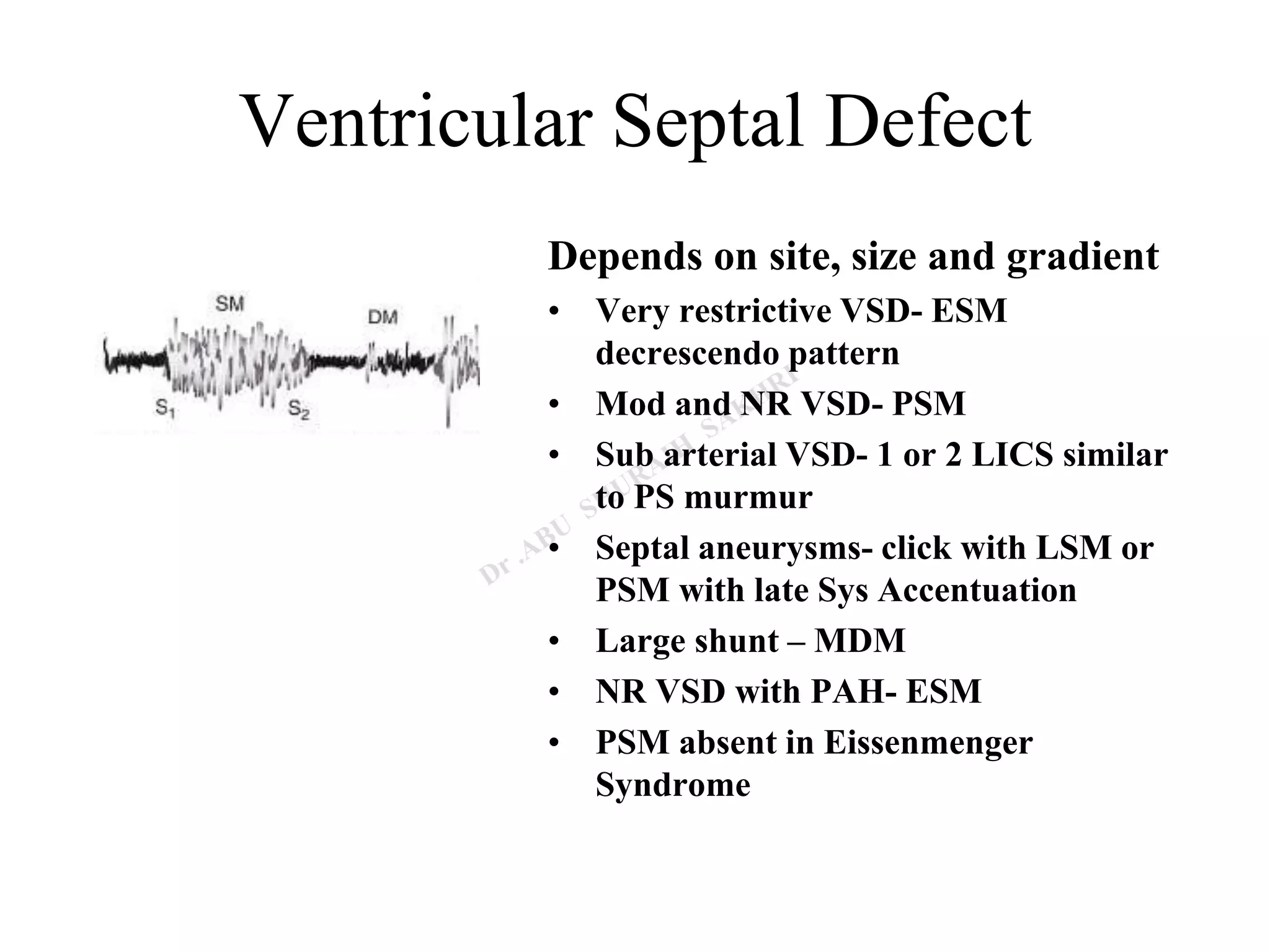
Heart murmurs can be produced by turbulence in blood flow caused by abnormalities in heart valves or structures. A murmur is described by its timing in the cardiac cycle, location, intensity, quality, and radiation pattern.
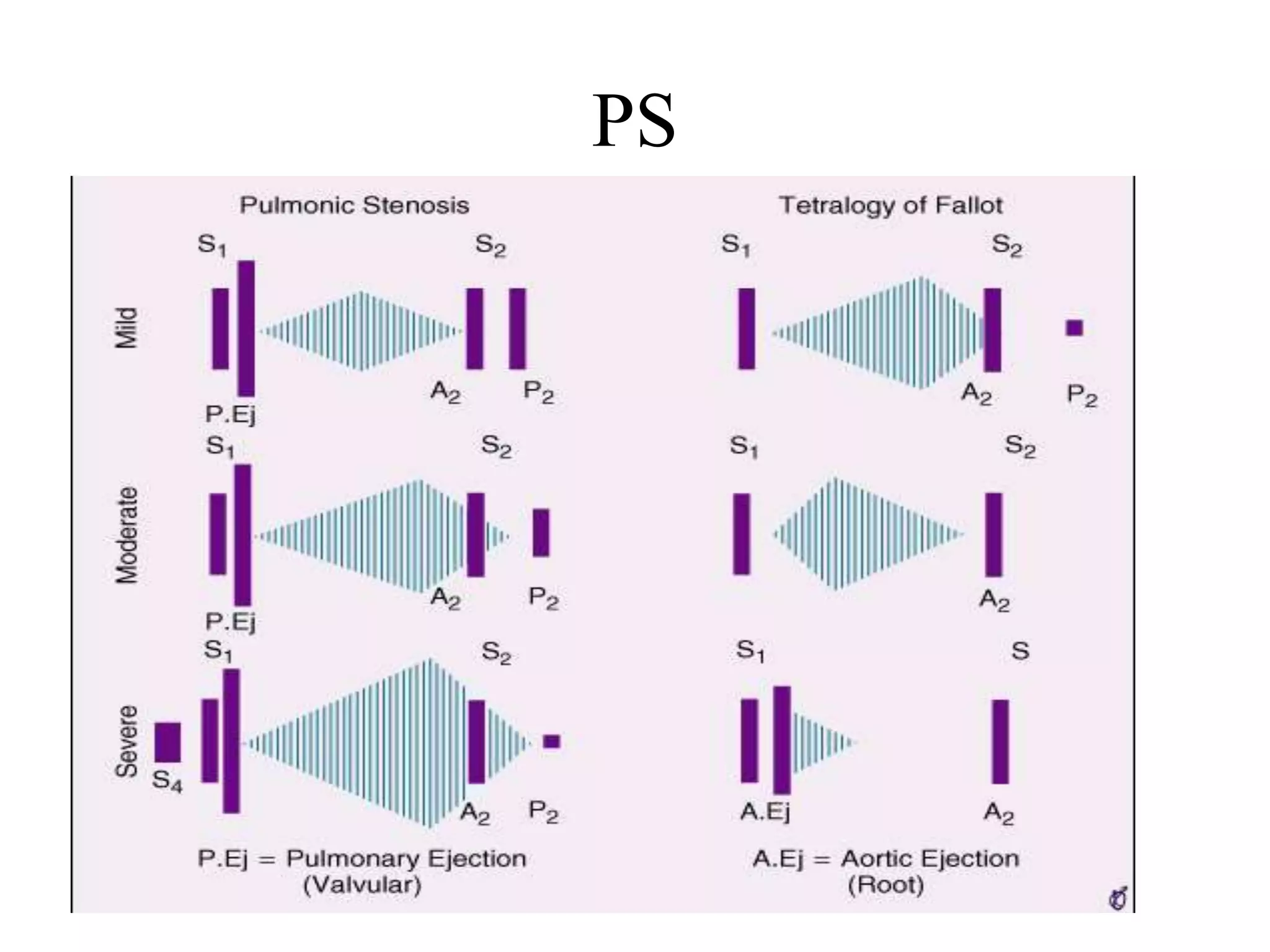
A mid-systolic murmur is the most common murmur and can be caused by ventricular outflow obstructions like aortic stenosis, dilation of the aorta/pulmonary trunk, accelerated flow, or innocent murmurs from normal anatomical variations. Diastolic murmurs include early diastolic murmurs like aortic regurgitation and high-pressure pulmonary regurgitation, and mid-diastolic murmurs caused by stenosis of the mitral or tricuspid valves. Flow murmurs




![How is a murmur produced?
L = linear dimension (internal
diameter In pipes)
V = mean fluid velocity
Q = volumetric flow rate
A = pipe cross-sectional area
m = dynamic viscosity of the fluid
n = kinematic viscosity [m/ r]
r = density of the fluid
Q = V1*A1= V2*A2
Q = P/R
[Re >4000 turbulent flow]
Re => Turbulence =>
murmur](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-5-2048.jpg)



![Description of a Murmur
• Position in the cardiac cycle
• Site of murmur [max. intensity]
• Intensity
• Quality & Pitch
• Conduction
• Dynamic changes](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-9-2048.jpg)










![AS
• Harsh, crescendo-decrescendo
MSM
• Early sys peak short duration vs.
Late systolic peak long duration
• Always Symmetrical [vs. PS]
• ES absent in calcific valves, sub
and supra valvular AS
• Length and loudness do not
necessarily corresponds to
severity but length more
suggestive of severity than other
murmurs
S4
Reverse
splitting S2](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-22-2048.jpg)
![AS
• Gallaverdin phenomenon/
hourglass phenomenon
Lower n (aortic) vs. Higher n
(mitral) periodic vibrations of stiffened
non calcific aortic valve
• Differentiating from MR
MR AS [ Gallaverdin]
Apical mid sys/ Holosystolic Apical mid sys
A2 buried in late sys
vibrations
Clear S2 heard
P/PVC unchanged P/PVC mur =
End of Long cycles in AF
unchanged
End of Long cycles
in AF =](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-23-2048.jpg)










![Physiological murmurs
Mammary Soufflé
• Late Pregnancy or puerperium
• Sometimes continuous louder in
systole, distinct gap from S1 [
time for ejected blood to reach
mammary arteries]
• 2 or 3 RICS/ LICS
• Light Pressure augments
murmur becomes continuous;
firm Pr abolishes murmur](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-35-2048.jpg)



![LSM
MVP
• Leaflets remains competent during early
ventricular contraction but overshoot in
late systole [critical V. dimensions]
• One or more mid systolic clicks precede
murmur [sudden deceleration of the
column of blood against the prolapsed
leaflet or scallops]
• Longer and softer
– Prompt standing after squatting
– Valsalva II
• Short & louder
– squatting
– Sustained hand grip
– Amyl nitrate
Other LSM- papillary muscle dysfunction
Post Pap Muscle . Late systolic cresendo to S2
Barlow’s syndrome refers to the
spectrum of symptoms caused by MVP
[click or murmur alone to palpitations,
chest pain, or syncope]](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-43-2048.jpg)

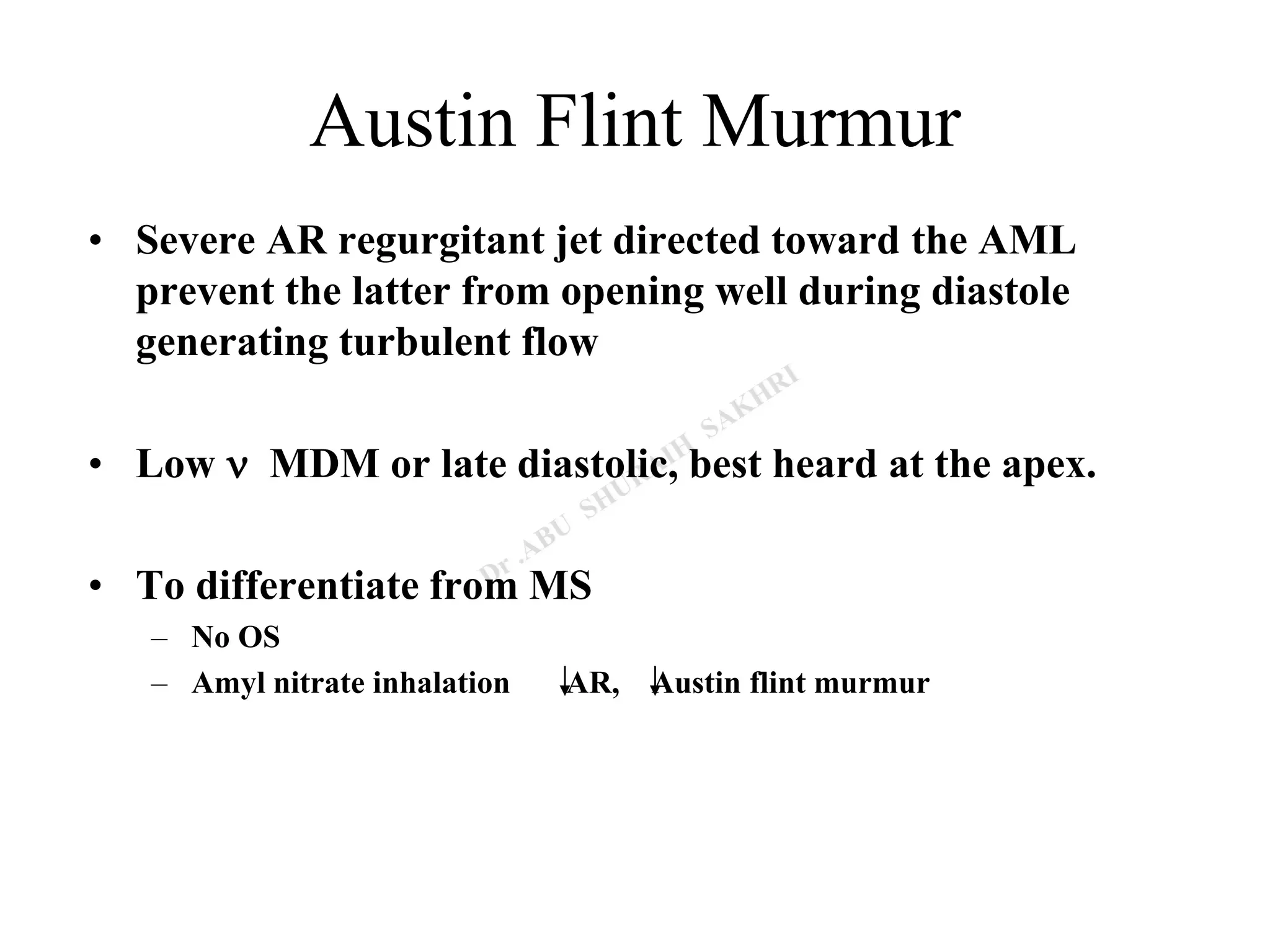
![Early diastolic murmur
• AR murmur
-Soft high frequency early diastolic
murmur with pt sitting & leaning
forward in full held expiration
-3 LICS [ 2 & 3 RICS in root dil]
-musical quality in eversion
-Austin Flint murmur
-Cole- Cecil murmur- AR murmur
in left axilla due to higher position of
apex](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-46-2048.jpg)

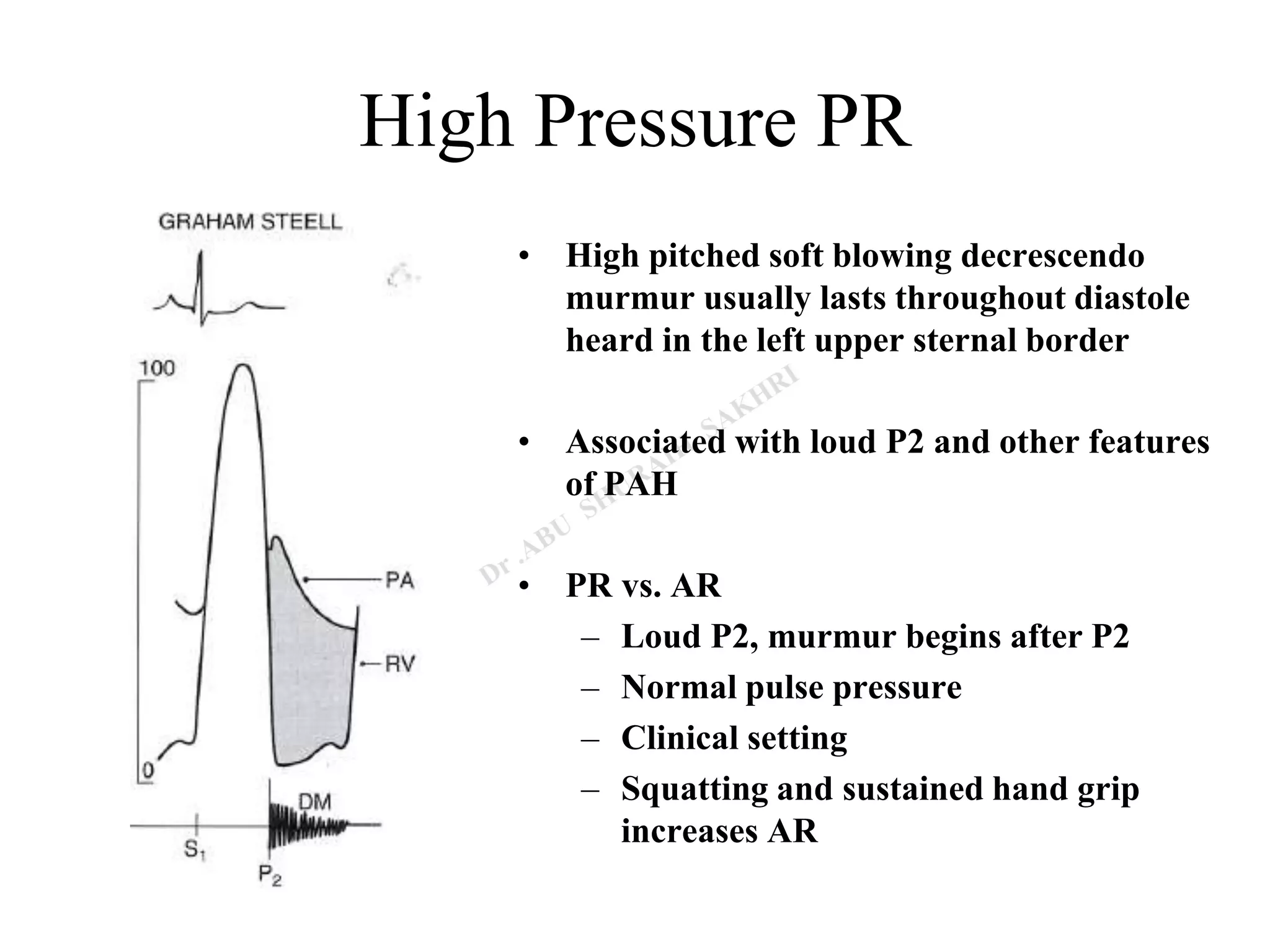

![Mid Diastolic Murmur
-Begin At Clear Interval After S2
I Rapid Filling Phase
Av valve obstruction Stenotic AV valves, tumors
Functional obstruction
Abnormal patterns of AV flow increased flow volume
increased flow velocity
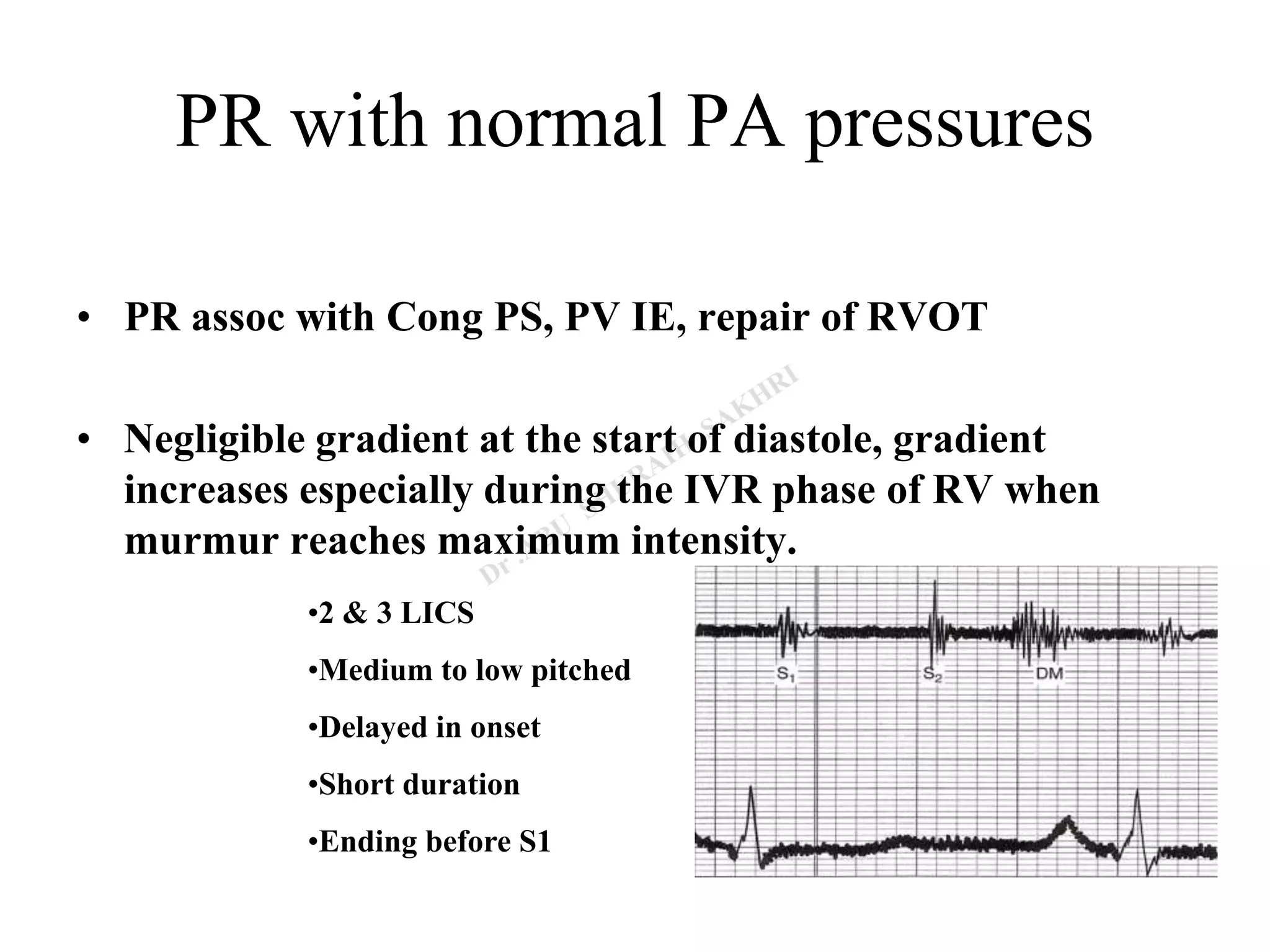
II Incompetent Pulmonary Valve [PR with normal PA
Pressure]
III Atherosclerotic extramural coronary arteries](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-50-2048.jpg)

![MS
• Low n rough rumbling [sound
of distant thunder] MDM
• Localized to apex, better heard
in left lateral position with bell
• Length a severity
• Long murmurs up to S1 even in
long cycles of AF- severe MS
• Late diastolic or Pre systolic
accentuation usually seen in
pliable valves and in NSR [
sometimes in AF]](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-52-2048.jpg)
![TS
• Similar to MS
• Murmur usually seen associated with AF
• Diff. from MS
– Increases during inspiration [Augmentation of RV volume, RV
Diastolic Pr., Flow rate and gradient across valve]
– LLSB](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-53-2048.jpg)
![Other Mid Diastolic Murmur
• Carey Coomb’s murmurs
– Acute rheumatic fever, mitral valve structures acutely inflamed with some
thickening and edema turbulence of flow during the rapid filling phase.
+ moderate MR [increased mitral inflow in diastole]
– Low pitched short MDM.
– good evidence of active carditis](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-56-2048.jpg)

![Late Diastolic/ Pre-systolic Murmurs
MS
• Higher frequency than MDM
• Sometimes only PSA heard- mild MS
• Generally absent in calcified valves and most of AF [ may
be present during short cycle lengths in AF]
• Cause-
– Increased flow during atrial contraction in late systole
– Increased dp/dt of LV contraction increases turbulence
[ esp. in AF short cycles]](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-58-2048.jpg)
![Other diastolic murmurs
• Cabot– Locke Murmur- [Diastolic Flow murmur]
– The Cabot–Locke murmur is a diastolic murmur that sounds similar to
aortic insufficiency but does not have a decrescendo; it is heard best at the
left sternal border. [High flow thru coronary vessels, LMCA, LAD]
– The murmur resolves with treatment of anaemia.
• Dock’s murmur
– diastolic crescendo-decrescendo, with late accentuation, [consistent with
blood flow through the coronary] in a sharply localized area, 4 cm left of
the sternum in the 3LICS, detectable only when the patient was sitting
upright.
– Due to stenosis of LAD](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-59-2048.jpg)
![Other diastolic murmurs
• Key–Hodgkin murmur
– EDM of AR; it has a raspy quality, [sound of a saw cutting through wood].
Hodgkin correlated the murmur with retroversion of the aortic valve
leaflets in syphilitic disease.
• Rytand’s murmur in complete heart block
– MDM or Late diastolic murmur
– Atrial contraction coincides with the phase of rapid diastolic filling
increased flow short MDM [intermittent].
– Another theory- Delayed V. contraction following A. contraction may lead
to diastolic MR & TR, because AV valve closure does not occur [unless V.
systole supervenes]. When higher V than A pressure during atrial
relaxation, an incompletely closed AV valve may lead to a reverse gradient
with a considerable regurgitation volume.](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-60-2048.jpg)



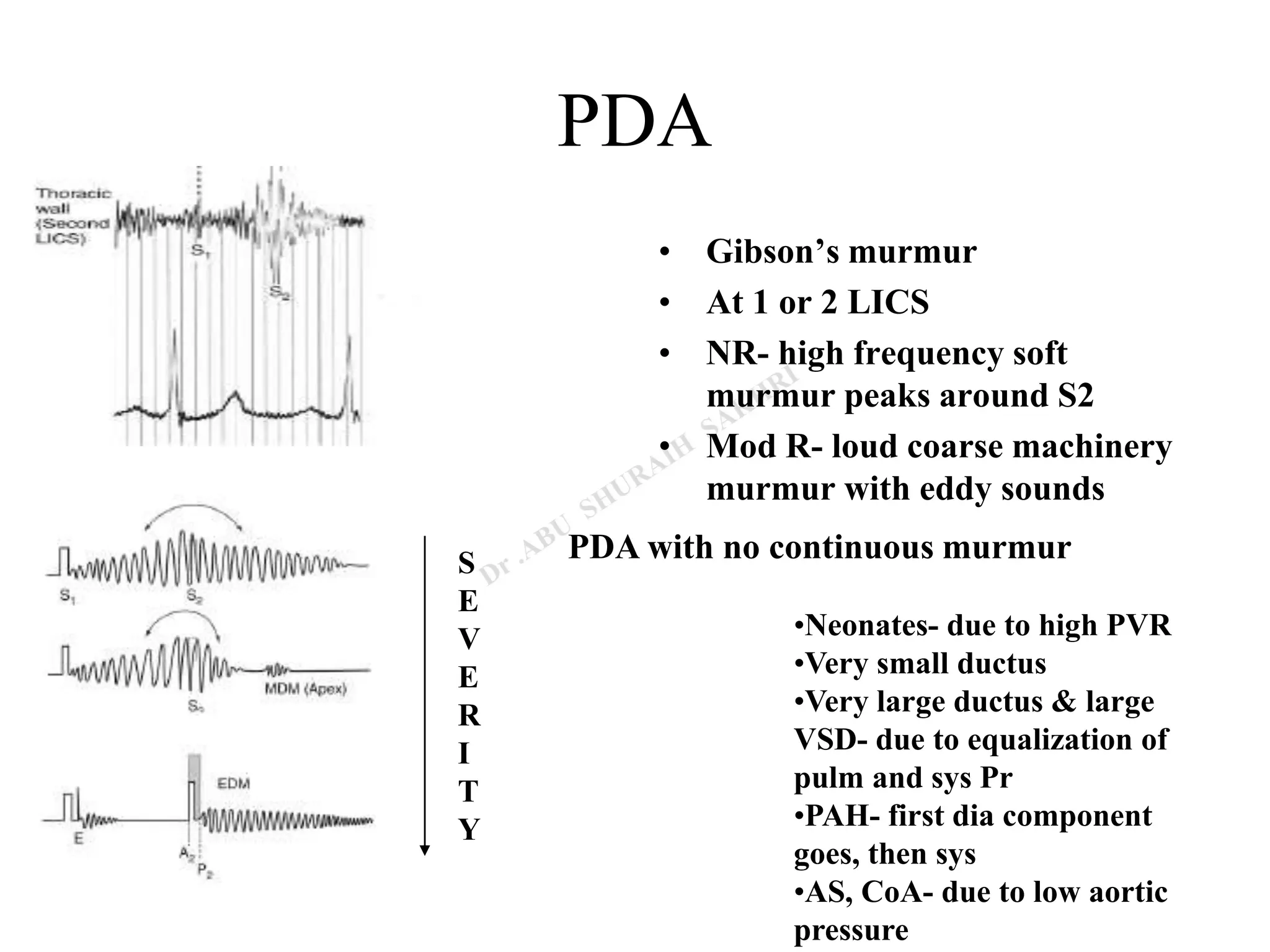
![Continuous murmurs
• APW
– 2 or 3 LICS
– Usually associated with early devp of eissenmenger
• RSOV
– No peaking at S2 seen [peaks in sys or dia.]
– To RA- RLSB
RV- LLSB
RVOT- 3 LICS
• Lutembacher syndrome with restricted ASD
– LLSB [body of RA]](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-65-2048.jpg)
![Continuous murmurs
• C-AVF
– RA- RLSB or RUSB
– CS- back b/w spine & Lt scapula
– RV inflow- LLSB
– RVOT- Upper to Mid LSB [beat to beat change in murmur may be
present, RV systolic compression, valsalva softens murmur]
– PA- ULSB [no eddy sounds]
• ALCAPA
– Murmur louder in diastole [LV contr. I/C flow]
– Do not peak at S2
– Usu LUSB or RUSB
-LA- ULSB rad to Lt ant ax line
- Lt SVC- upper to mid LSB](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-66-2048.jpg)




![Position
A. Lt Lateral Decubitus
LV impulse [apical sounds, murmurs better heard]
Act of turning increases HR[ MDM & PSA of MS ],
induces PVC [AS murmur vs. MR murmur (n/c)]
B. Sitting leaning forward full held expiration
AR & PR EDM
C. Sitting with legs dangling
Further reduces venous return
If S2 fails to fuse on sitting
D. Elbow Knee Position
Pericardial friction rub](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-72-2048.jpg)
![Position
E. Standing to squatting and vice versa
– Standing[ venous return, BP ]; [opp. in squatting]
1. All murmurs [except HOCM , MVP earlier]
• HOCM [ LV contractility, after load, preload]
• MVP [ preload, afterload ]
2. A2- P2 , A2-OS , A2-S3 (n/c)
F. Hyperextension of shoulders
supraclavicular Systolic murmurs
G. Stretching of Neck
Venous hum
H. Passive elevation of both legs
Transiently increases venous return, increase S3](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-73-2048.jpg)
![Physical Maneuvers
Inspiration
• Right sided events become more
prominent
• S2 split appreciable
• RVs3 RVs4 prominent
• Tricuspid sys & dia Mur
increased
• Pulm ejection sound reduced
Expiration
• Left sided events become more
prominent
• Diff AR & PR
• Pericardial friction rub
[exhalation & supine]
• Innocent pulm mid sys murmur
becomes more prominent becos
of reduced AP diameter](https://image.slidesharecdn.com/heartmurmurs-220112165124/75/HEART-MURMURS-74-2048.jpg)