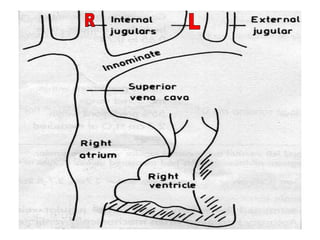
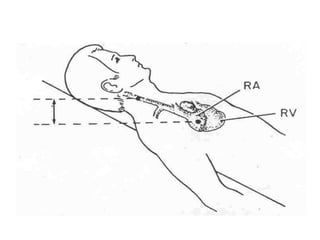
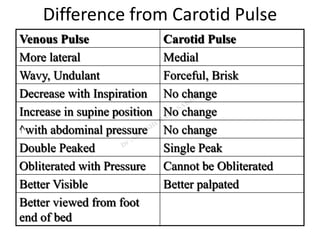
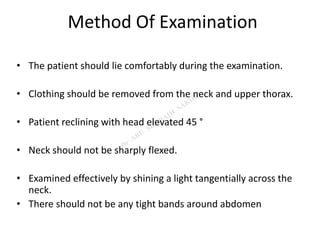
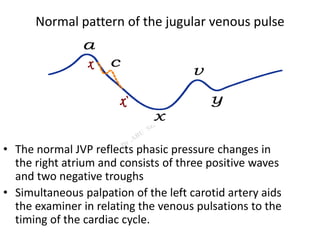
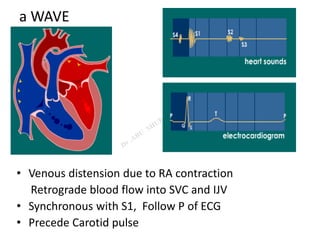
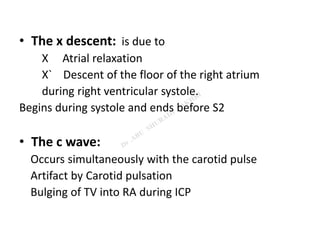
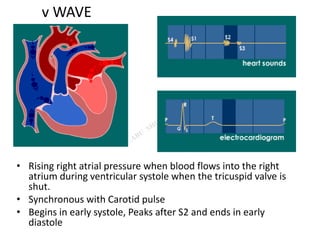
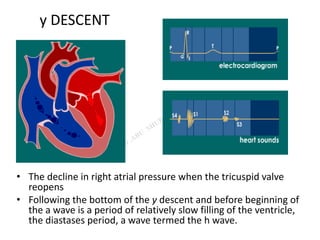
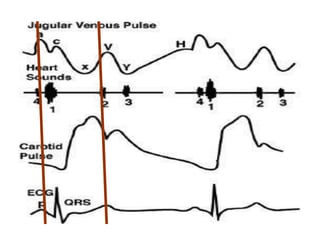
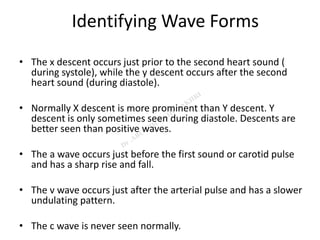
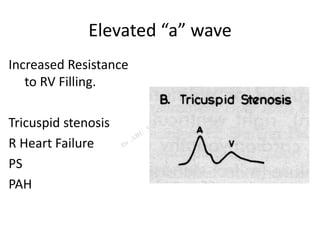
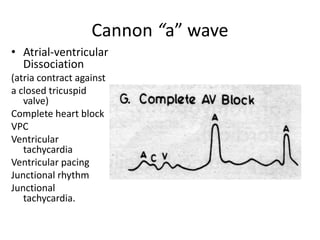
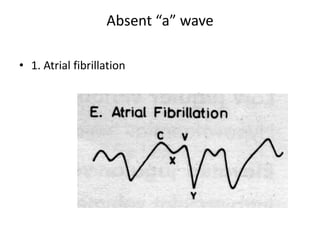
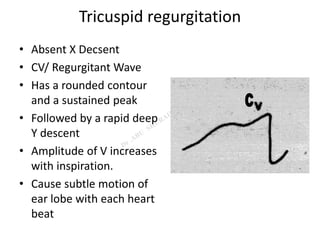
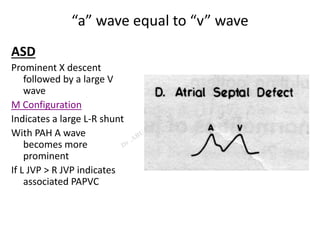
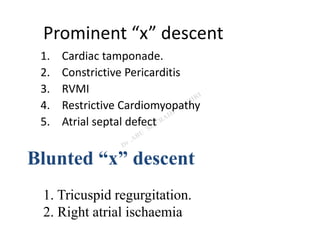
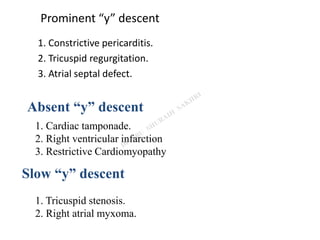
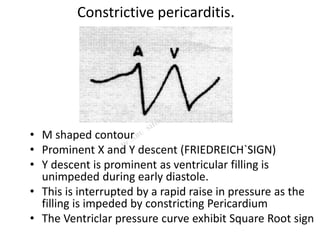
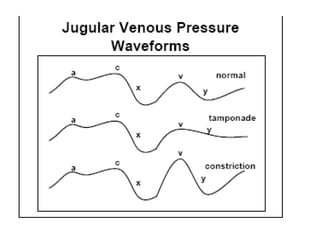
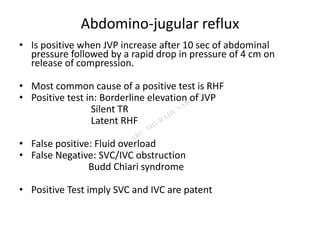
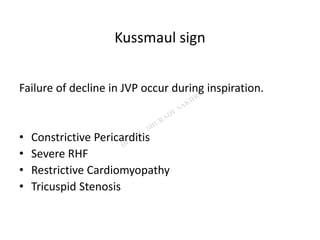
The jugular venous pulse reflects right atrial pressure and is best examined in the right internal jugular vein. It normally displays three positive waves and two negative troughs related to atrial filling and emptying. Abnormalities can indicate conditions that elevate or lower right atrial pressure such as heart failure, tamponade, constriction. Specific wave changes suggest problems like tricuspid regurgitation or stenosis. The jugular venous pulse is a useful physical exam finding for cardiovascular assessment.