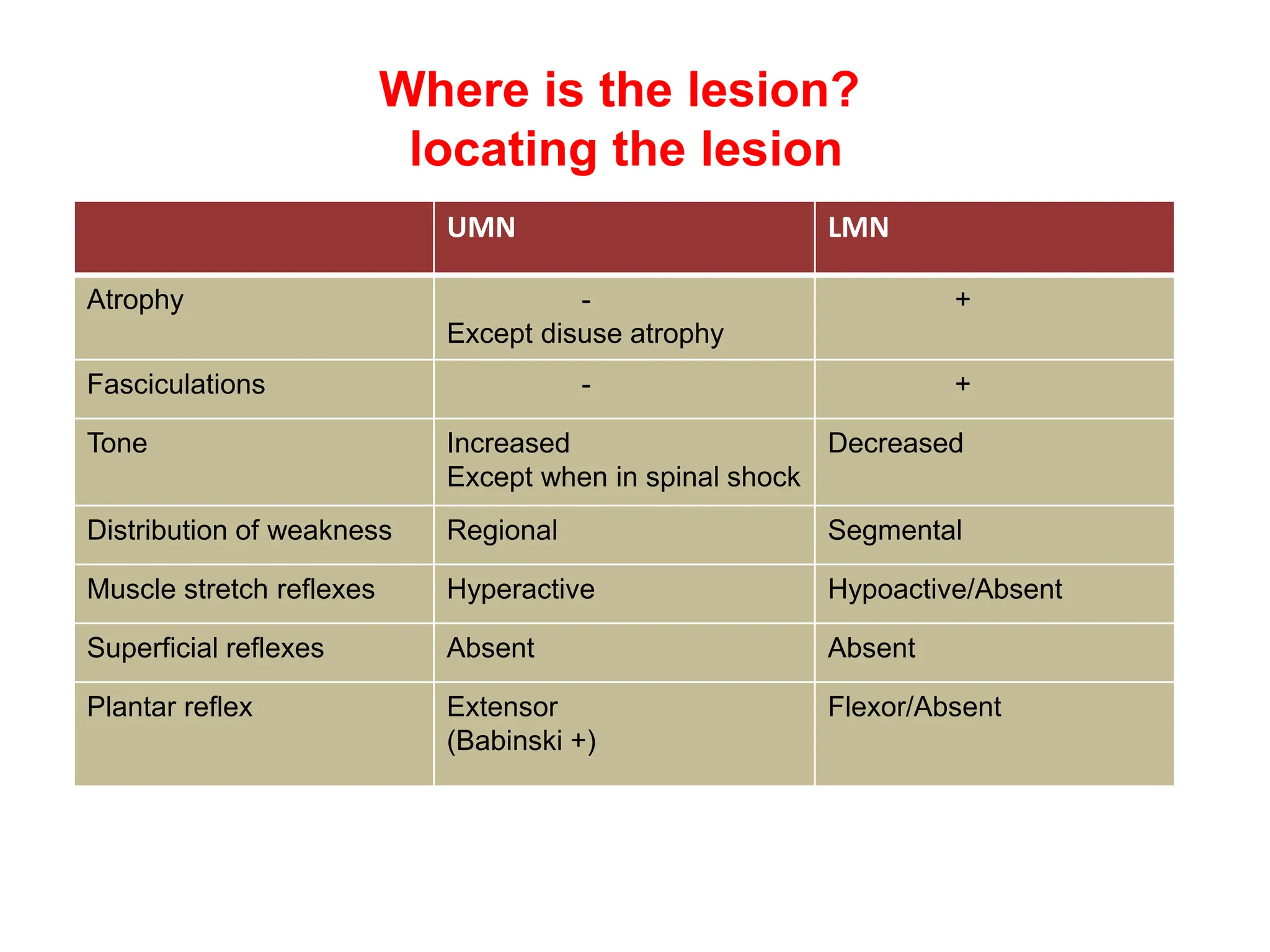
The document discusses various forms of neurological weakness, their classifications, causes, and characteristics as measured by muscle power and reflex activity. It distinguishes between upper motor neuron (UMN) and lower motor neuron (LMN) lesions, examining the differing effects on muscle tone, reflexes, and overall strength. Additionally, it outlines the diagnostic approach to assessing weakness, including the use of imaging and electrophysiological studies, while also covering specific conditions and their implications for muscle weakness.