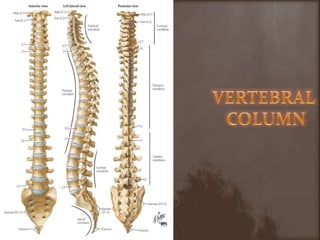
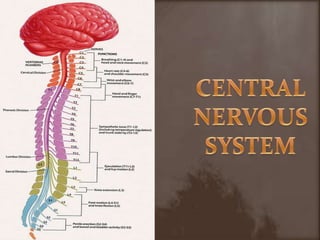
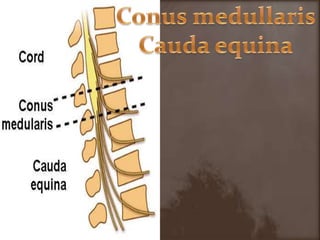
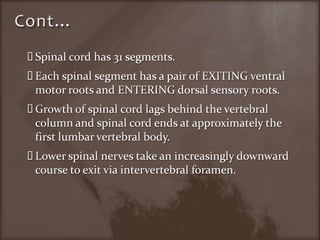
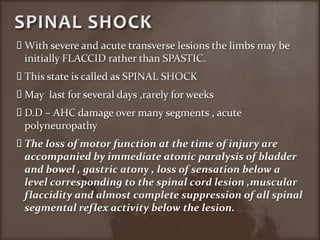
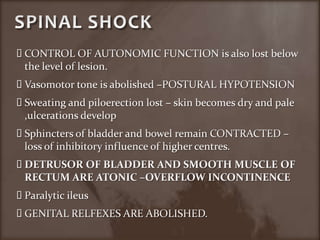
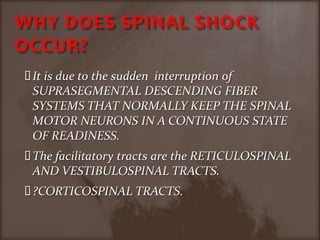
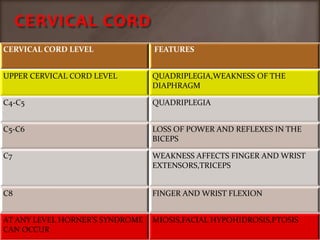
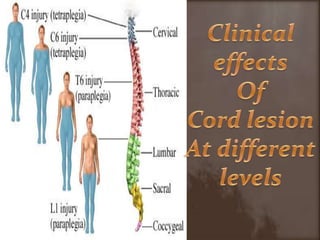
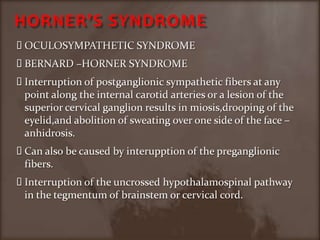
1. The document discusses various types of spinal cord injuries including paraplegia, quadriplegia, and different syndromes that can result from lesions at specific levels of the spinal cord such as cervical, thoracic, lumbar, and conus medullaris.
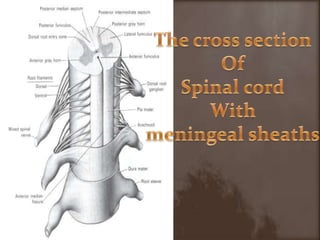
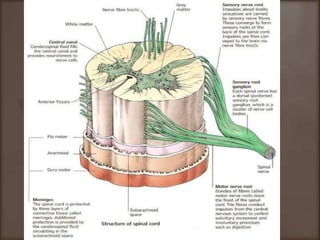
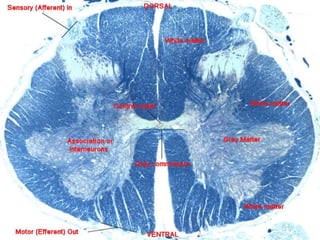
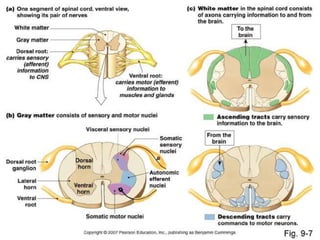
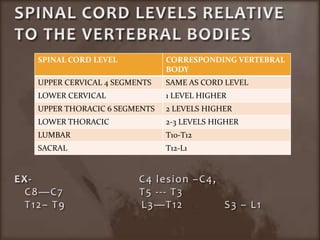
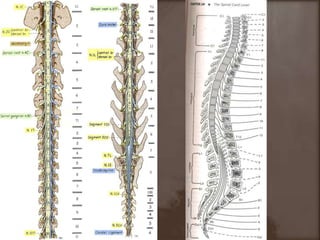
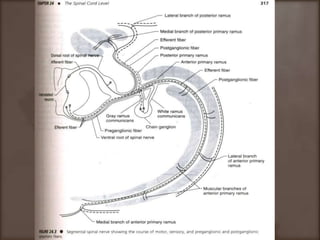
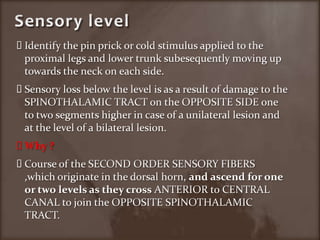
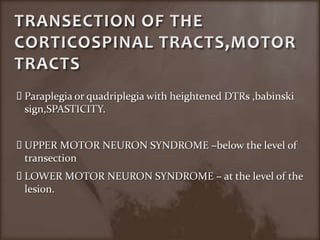
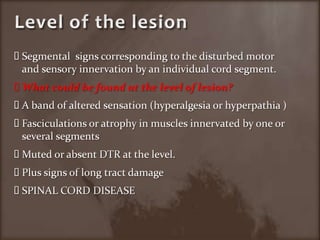
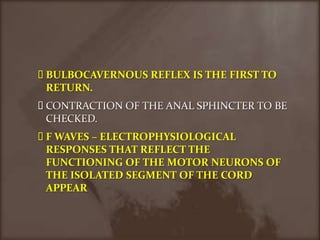
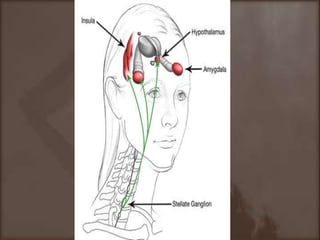
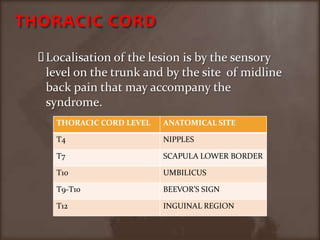
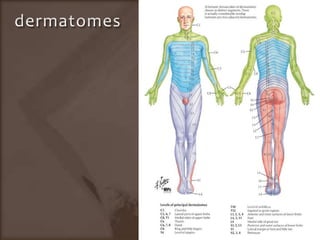
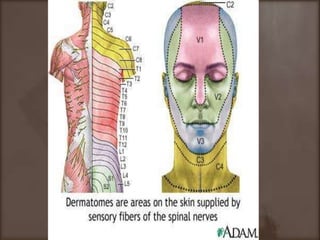
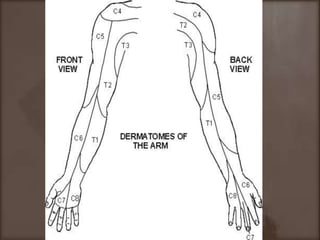
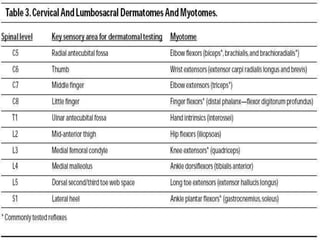
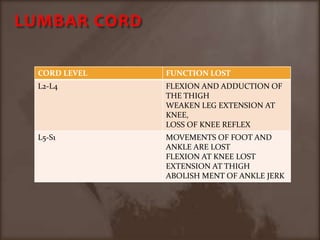
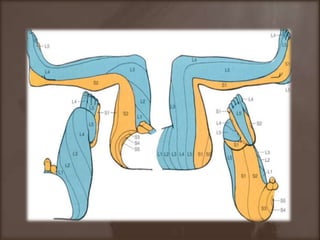
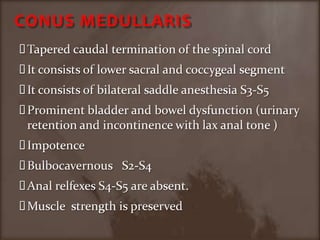
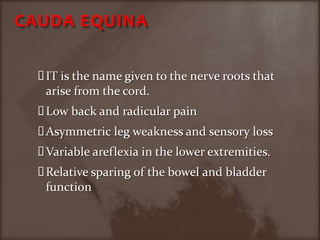
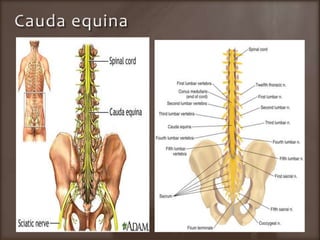
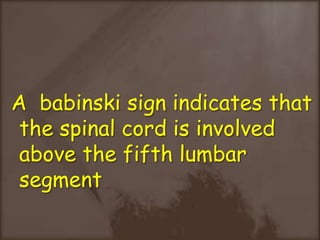
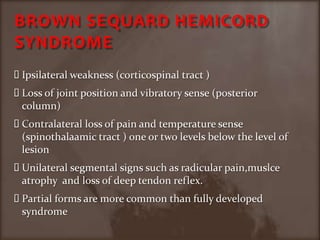
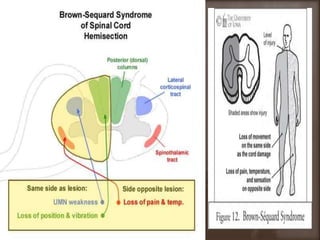
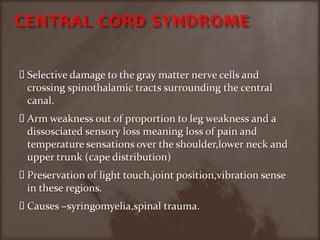
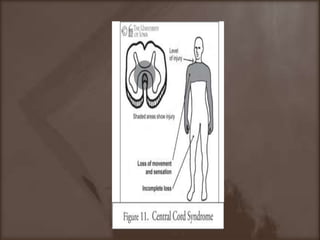
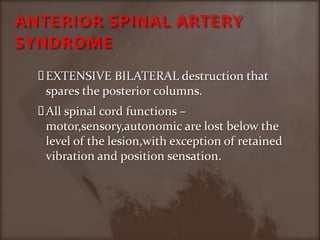
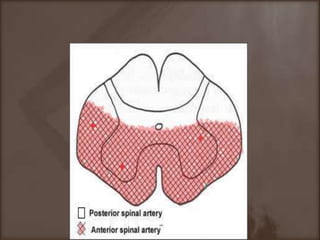
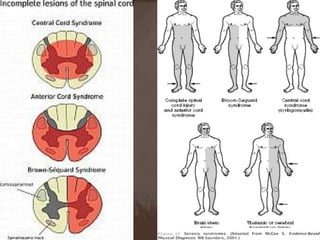
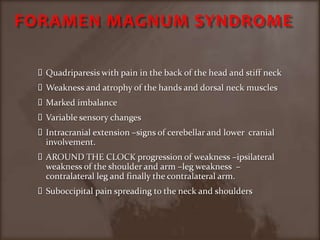
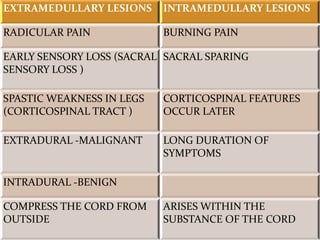
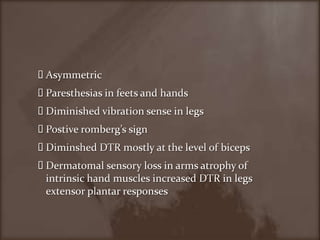
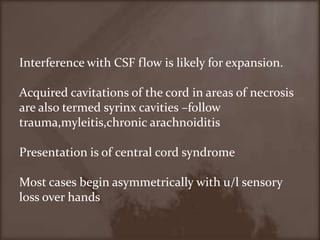
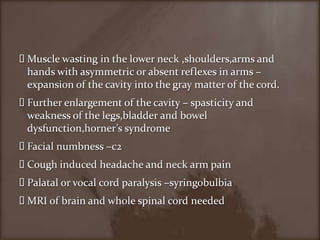
2. It describes how to determine the level of a spinal cord lesion based on assessing the sensory level and signs of motor and autonomic dysfunction. Syndromes like Brown-Sequard and central cord are also summarized.
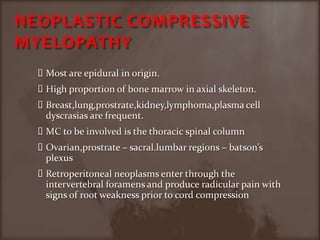
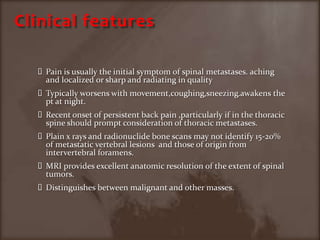
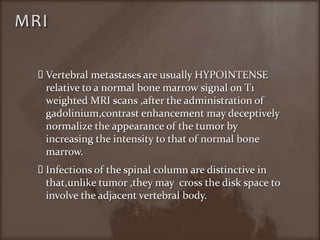
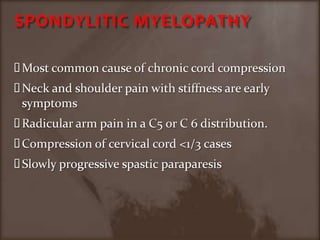
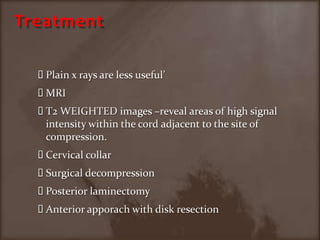
3. Common causes of compressive myelopathy include neoplastic etiologies with metastases most often occurring in the thoracic region.