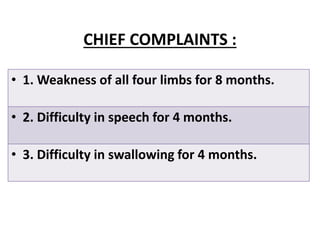
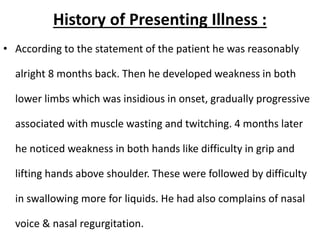
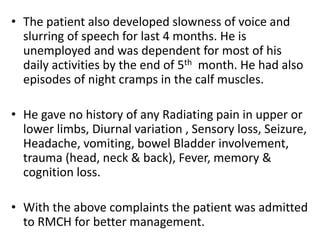
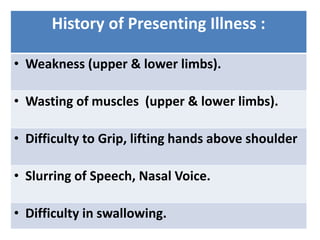
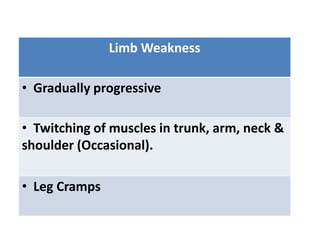
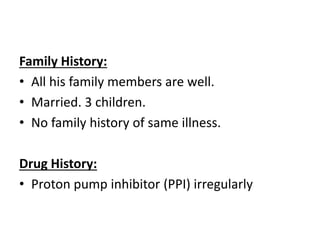
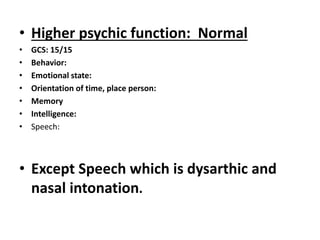
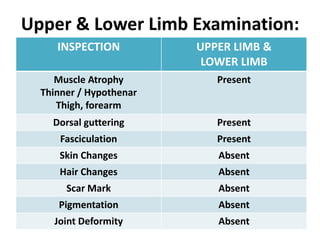
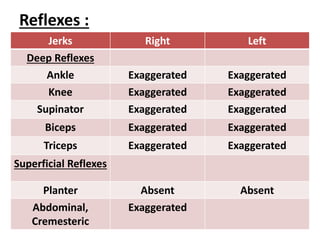
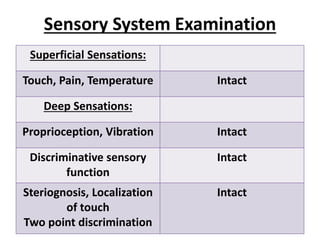
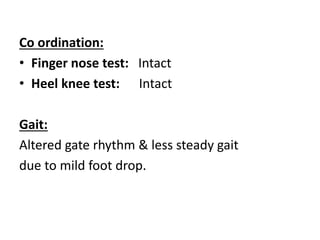
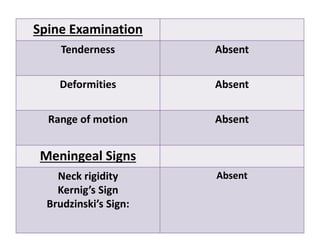
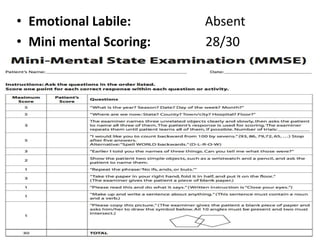
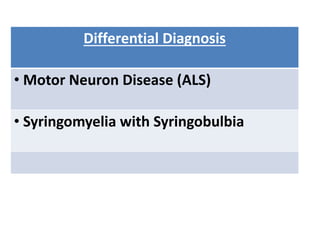
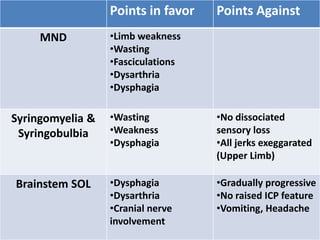
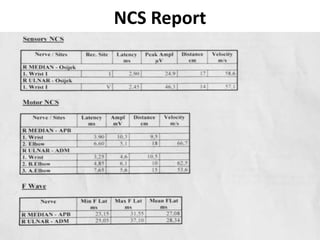
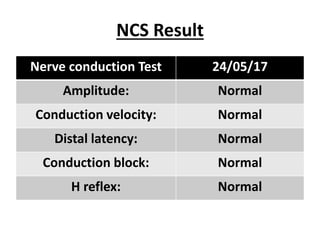
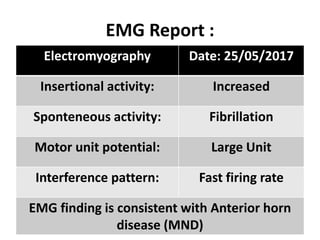
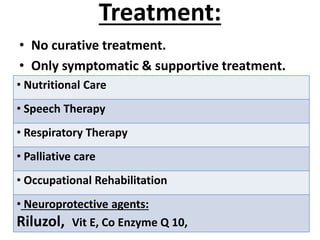
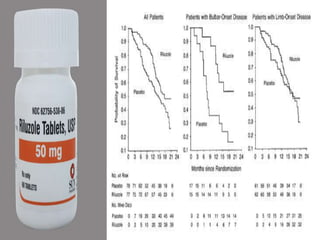
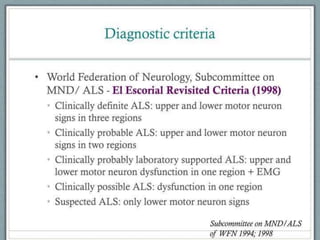
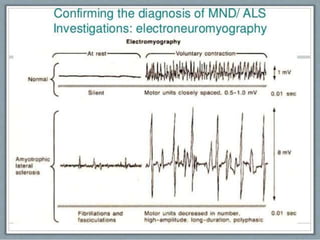
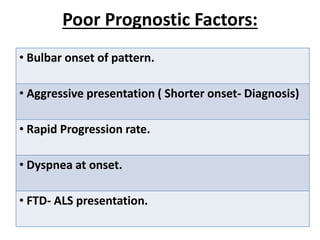
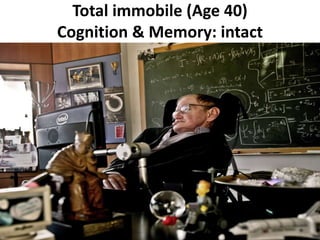
This document summarizes the case of a 48-year-old man who presented with weakness in all four limbs for 8 months and difficulty with speech and swallowing for 4 months. On examination, he had muscle wasting and increased tone in his limbs as well as dysarthria and slurred speech. Investigations including MRI, NCS, and EMG were consistent with a diagnosis of motor neuron disease (ALS). He was started on supportive treatment for ALS but the prognosis for this progressive disorder is fatal within 3-5 years in most cases.