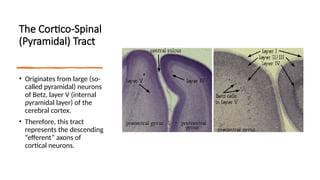
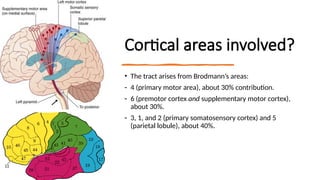
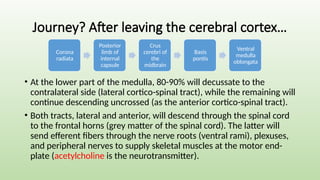
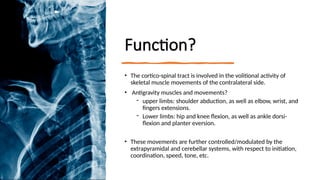
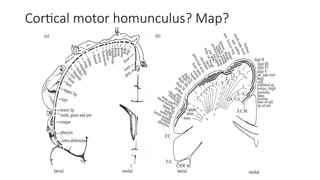
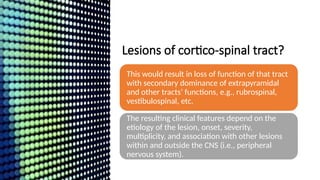
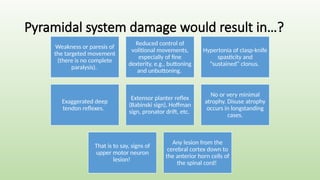
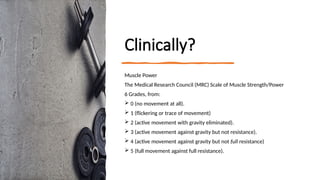
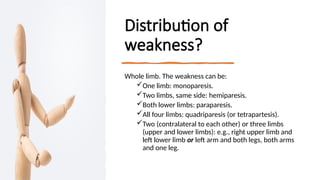
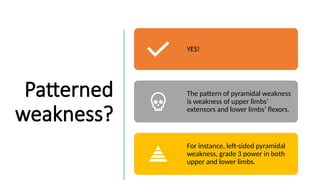
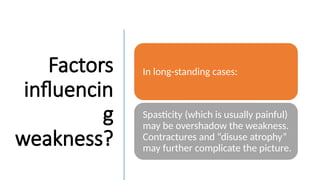
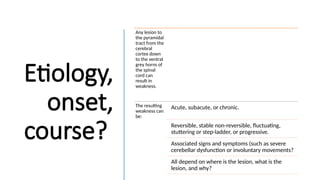
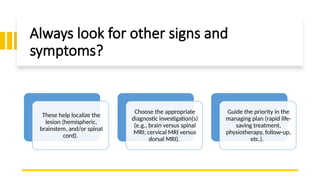
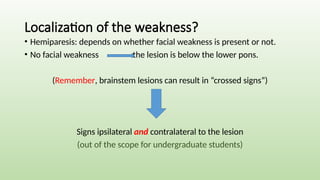
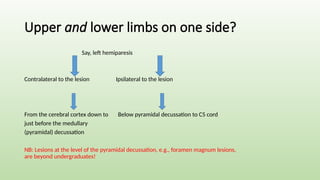
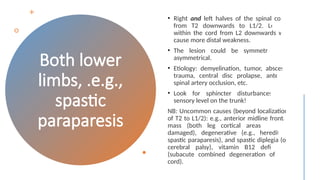
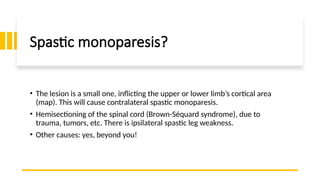
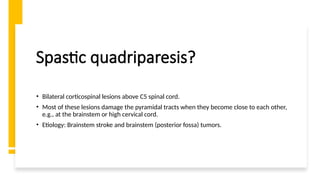
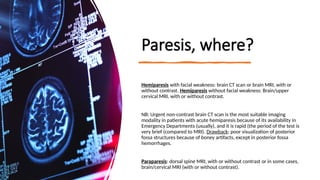
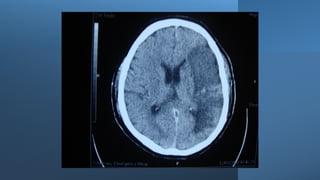
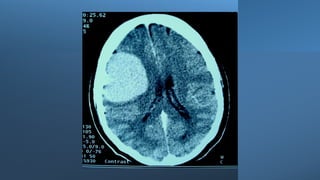
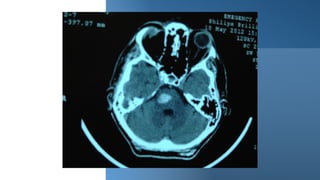
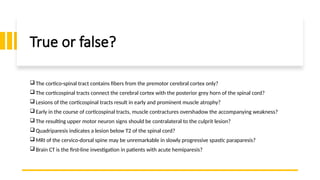
This document outlines the anatomy and function of the cortico-spinal tract, detailing its role in upper motor neuron lesions and associated clinical features such as weakness and reflex changes. It covers the etiology of weakness, types of paresis, diagnostic approaches, and treatment strategies for upper motor neuron damage. Additionally, it discusses the medical research council scale for muscle strength and the implications of various neurological examinations in diagnosing conditions related to the cortico-spinal tract.