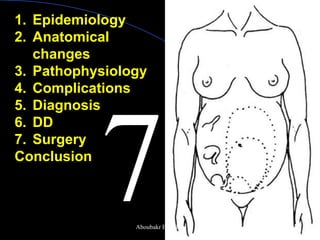
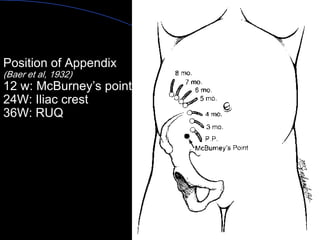
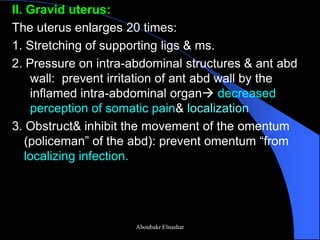
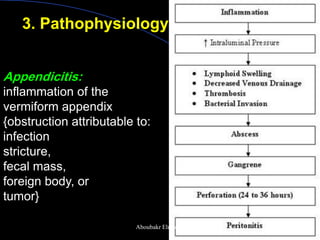
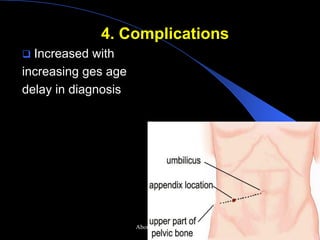
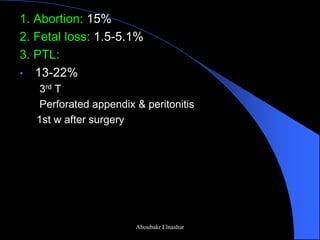
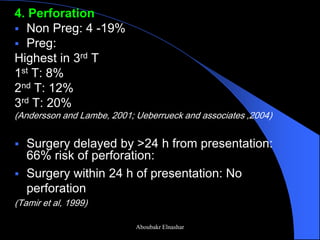
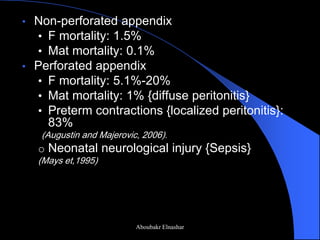
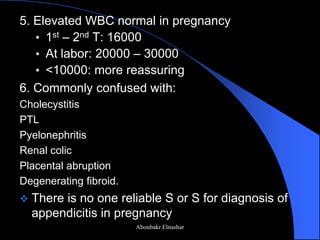
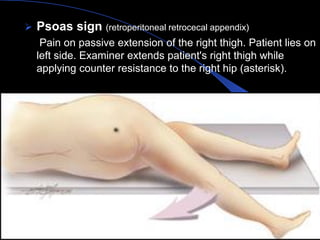
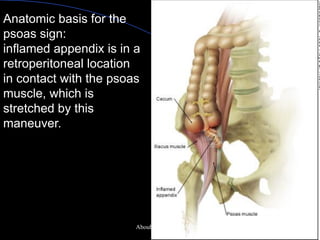
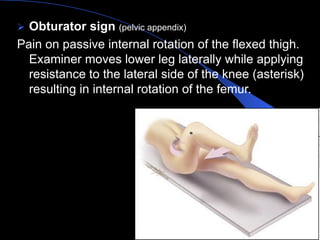
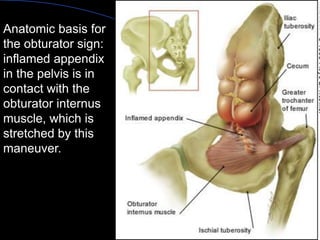
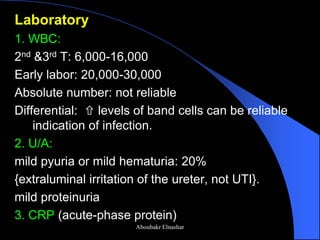
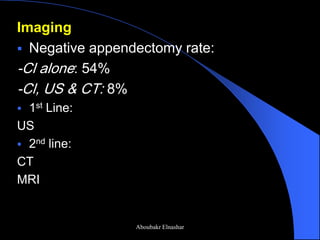
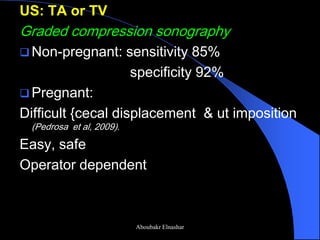
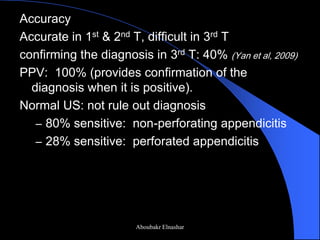
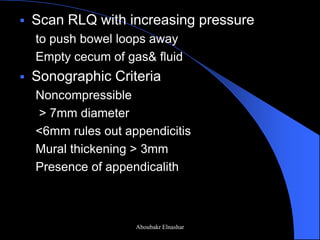
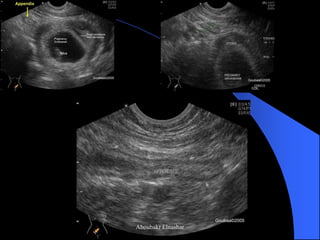
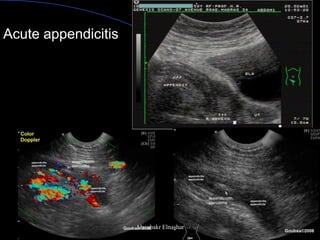
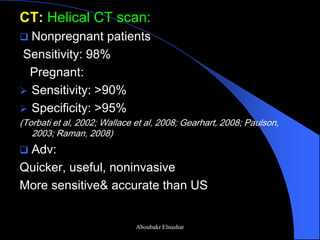
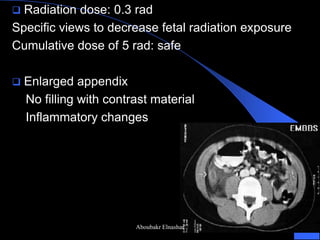
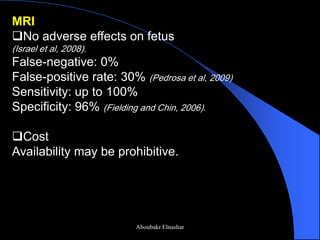
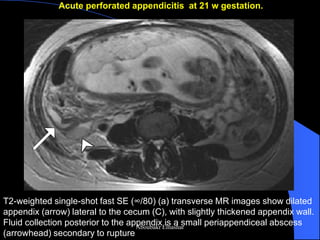
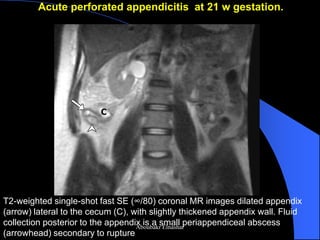
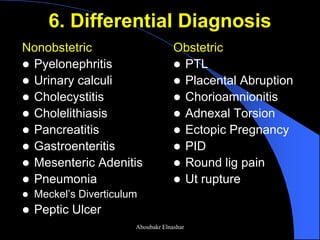
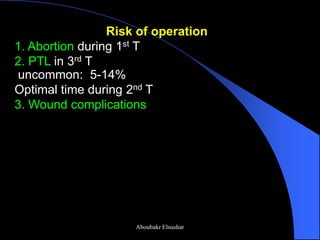
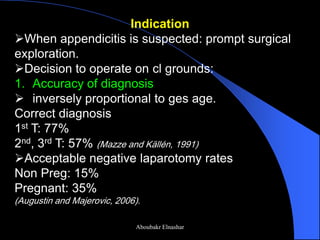
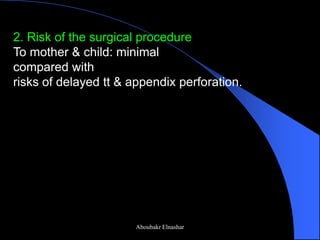
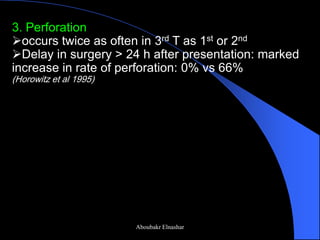
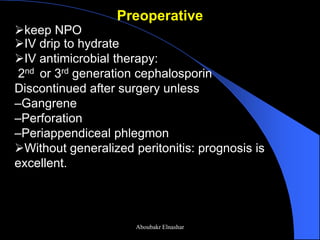
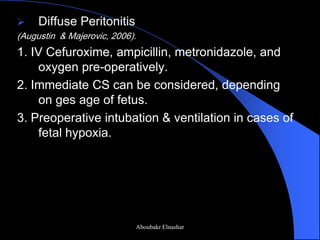
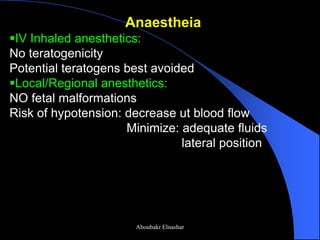
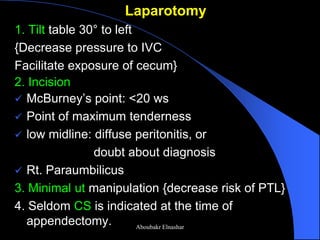
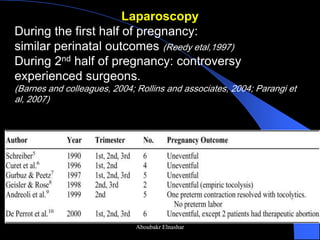
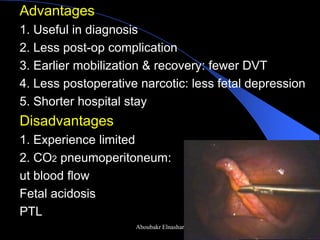
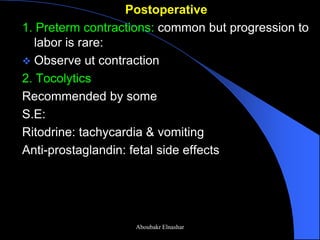
This document discusses appendicitis during pregnancy. It covers the epidemiology, anatomical changes, pathophysiology, complications, diagnosis, differential diagnosis, and surgery of appendicitis in pregnant patients. The key points are that appendicitis occurs in about 1 in 1500 pregnancies, symptoms can be more difficult to diagnose due to pregnancy-related changes, ultrasound and CT scan are used for diagnosis but have limitations during late pregnancy, and prompt surgical treatment is indicated to prevent complications of perforation for both the mother and fetus.