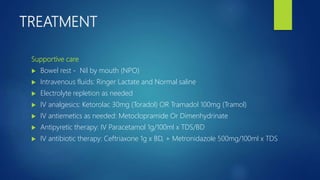
Acute appendicitis is defined as inflammation of the vermiform appendix, categorized as uncomplicated or complicated based on the presence of additional issues such as perforation or fecalith. Common causes include obstruction due to lymphoid hyperplasia in younger patients and fecaliths in adults, leading to symptoms like abdominal pain, nausea, and fever. Treatment typically involves supportive care and antibiotics, with appendectomy being the standard surgical intervention for non-perforated cases.