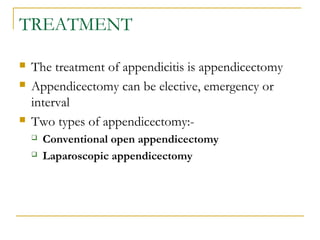
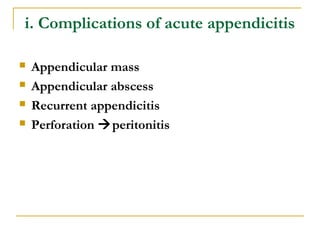
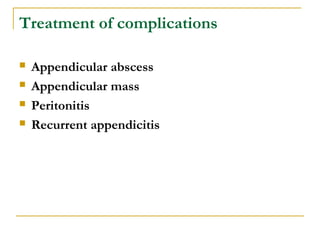
This document defines appendicitis and provides details about its historical perspective, epidemiology, etiology, classification, pathophysiology, clinical presentation, differential diagnosis, workup, treatment, and complications. Specifically, it notes that appendicitis is inflammation of the vermiform appendix and was first described in 1886. It occurs most commonly in the second and third decades of life and has a higher incidence in males. Obstruction of the appendix is a major cause and results in increased intraluminal pressure and bacterial overgrowth. Clinical presentation involves shifting pain from the periumbilical region to the right lower quadrant. Treatment is an appendectomy, which can be open or laparoscopic. Complications include appendiceal
![EPIDEMIOLOGY [cont’d]
Mortality/Morbidity:
The overall mortality rate of 0.2-0.8% is attributable to
complications of the disease rather than to surgical intervention
Mortality rate rises above 20% in patients older than 70 years,
primarily because of diagnostic and therapeutic delay
Perforation rate is higher among patients younger than 18 years
and patients older than 50 years, possibly because of delays in
diagnosis
Appendiceal perforation is associated with an increase in
morbidity and mortality rates](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-6-320.jpg)
![EPIDEMIOLOGY [cont’d]
Sex:
The incidence of appendicitis is approximately 1.4 times
greater in men than in women
The incidence of primary appendectomy is approximately
equal in both sexes](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-7-320.jpg)
![EPIDEMIOLOGY [cont’d]
Age:
Appendicitis may occur at all ages, but is most commonly
seen in the 2nd
and 3rd
decades of life
The incidence of appendicitis gradually rises from birth,
peaks in the late teen years, and gradually declines in the
geriatric years
Although rare, neonatal and even prenatal appendicitis
have been reported in literature
The emergency physician must maintain a high index of
suspicion in all age groups](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-8-320.jpg)
![Obstructive appendicitis
Luminal obstruction and mucus production result in
increased intraluminal pressure
Bacteria trapped within the appendiceal lumen begin to
multiply, and the appendix becomes distended
Luminal distention stimulates visceral nerve endings
concerned with pain [visceral pain]
This produce dull aching pain felt periumbilically
according to nerve supply of the appendix (T10)
referred pain
Venous congestion and edema follow next, and by 12 hours
after onset, the inflammatory process may become
transmural](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-17-320.jpg)
![Obstructive appendicitis[ cont]
Peritoneal irritation then develops
If the obstruction is left untreated, arterial blood
flow to the appendix is compromised, and this
leads to tissue ischemia and necrosis
This stimulates parietal nerve endings→ shift of
pain to the RIF
Full thickness necrosis of the appendiceal wall
leads to perforation with the release of fecal and
suppurative contents into the peritoneal cavity](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-18-320.jpg)
![Obstructive appendicitis [cont]
Depending on the duration of the disease process,
either a localized walled-off abscess or mass occurs,
or if the pathologic process has advanced rapidly, the
perforation is free in the peritoneal cavity and
generalized peritonitis occurs
The commonest bacterial growth from inflamed
appendices include Escherichia coli, Kleblesiella
spp., Proteus spp and Bacteroids](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-19-320.jpg)
![CLINICAL PRESENTATION
History: classic symptoms include:-
Periumbilical pain [visceral pain] which shifts and
localize to the RIF [parietal or somatic pain]
Periumbilical pain is colicky in nature in obstructive type
and is dull aching and constant in non-obstructive type
RIF pain is sharp intense and well localized to the RIF
Anorexia
Nausea & Vomiting](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-21-320.jpg)
![CLINICAL PRESENTATION [cont’d]
Physical examination
Pyrexia
RIF tenderness
Muscle guarding
Rebound tenderness
Special test to elicit in appendicitis
Pointing sign
Rovsing’s sign [RIF pain with palpation of the LIF ]
Psoas sign [RIF tenderness with internal rotation of the flexed
right hip]
Obtrurator sign [RLQ pain with hyperextension of the right hip ]](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-22-320.jpg)
![WORK UP [cont’d]
Imaging investigations
Abdominal radiography
The kidneys-ureters-bladder (KUB) view is typically used
Visualization of an appendicolith in a patient with symptoms
consistent with appendicitis is highly suggestive of appendicitis,
but this occurs in fewer than 10% of cases
The consensus in the literature is that plain radiographs are
insensitive, nonspecific, and is not cost-effective
•](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-30-320.jpg)
![WORK UP [cont’d]
Abdominal Ultrasonography
An outer diameter of greater than 6 mm,
noncompressibility, lack of peristalsis, or
periappendiceal fluid collection characterizes an
inflamed appendix
The normal appendix is not visualized
It’s noninvasive, short acquisition time, lack of
radiation exposure, and potential for diagnosis of
other causes of abdominal pain, particularly in the
subset of women of childbearing age
However it is operator dependent](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-31-320.jpg)
![WORK UP [cont’d]
Computed tomography
Abdominal CT has become the most important imaging study in the
evaluation of patients with atypical presentations of appendicitis
Advantages of CT scanning include
Sensitivity and accuracy compared with those of other imaging
techniques
Readily available
Noninvasive
potential to reveal alternative diagnoses
Disadvantages
lengthy acquisition time if oral contrast is used
patient discomfort if rectal contrast is used
Exposure to radiation
It is really required to make diagnosis of acute appendicitis](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-32-320.jpg)
![DIAGNOSTIC SCORING SYSTEM
Various scoring systems have been devised to aid diagnosis
of appendicitis
Although many diagnostic scores have been advocated,
most are complex and difficult to implement in the clinical
situation
The Alvarado score, is a simple scoring system that can be
instituted easily
The Classic Alvarado score [1986] is based on three
symptoms, three signs and two laboratory findings and has
a total score of 10](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-33-320.jpg)
![Classic Alvarado Score [1986]
Features Score
Symptoms
Migratory RIF pain 1
Anorexia 1
Nausea & vomiting 1
Signs
Pyrexia 1
Tenderness RIF 1
Rebound tenderness RIF 2
Lab investigations
Leucocytosis 2
left shift of neutrophil maturation 1
Total 10](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-34-320.jpg)
![Diagnostic Scoring System [cont]
Kalan et al [1994] omitted one lab parameter [left
shift of neutrophil maturation] which is not
routinely available in many laboratories, and
produced a modified score which have only one
lab findings
A modified Alvarado score [1994] is based on three
symptoms, three signs and one laboratory findings
[total score of 9]
MAS is commonly used](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-35-320.jpg)
![Modified Alvarado Score [1994]
Features Score
Symptoms
Migratory RIF pain
Anorexia
Nausea & vomiting
1
1
1
Signs
Pyrexia
Tenderness RIF
Rebound tenderness RIF
Lab investigation
leucocytosis
1
1
2
2
Total 9](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-36-320.jpg)
![MASS- interpretation
A score of 1-4:[ discharging group] The diagnosis
of acute appendicitis is unlikely
A score of 5-6: [observing group] Probable to have
appendicitis but not convincing to have urgent
appendicectomy
A score of 7-9: [emergency group] Regarded as
probable to have acute appendicitis and needs
emergency appendicectomy](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-37-320.jpg)
![Intraoperative care
Open appendicectomy
Incisions
Grid-iron sss
Rurtherford Morrison’s
Lanz’s [transverse skin crease]
SUMI when the diagnosis is not clear
Rt lower paramedian
Midline incision](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-40-320.jpg)
![Intraoperative care cont’d
Appendiceal locations of the tip
Retrocaecal appendix [70%]
Pelvic appendix [25%]- the tip hangs in the pelvic brim
Subcaecal appendix [2%]
Splenic appendix [1%]- either pre- or post-ileal i.e anterior or
posterior to the terminal ileum
Paracaecal appendix [1%]
Paracolic appendix [1%]-either to the right or left of ascending
colon, the tip in the extraperitoneal tissue
Location of the base-is constant, being found at
confluence of 3 taeniae coli of the caecum which fuse to
form the outer longitudinal muscle coat of the appendix](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-41-320.jpg)
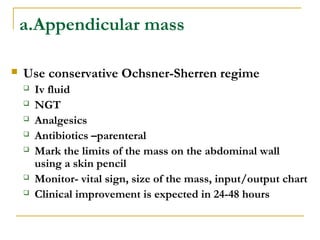
![Appendicular mass [cont]
Criteria for stoping OSR
Increased pulse rate
Increasing or spreading abdominal pain
Increasing the size of the mass
Vomiting or increasing gastric contents](https://image.slidesharecdn.com/03-150427073915-conversion-gate01/85/03-appendicitis-dr-phillip-bmc-47-320.jpg)