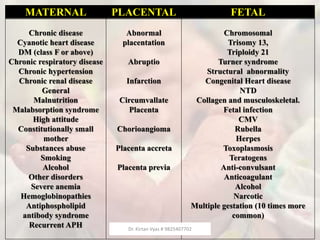
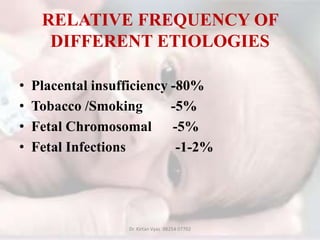
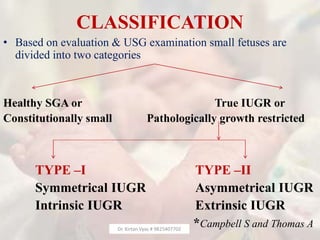
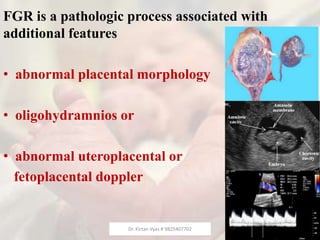
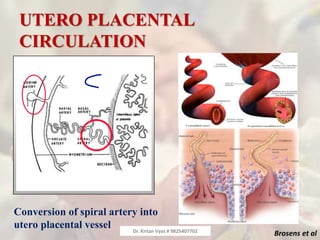
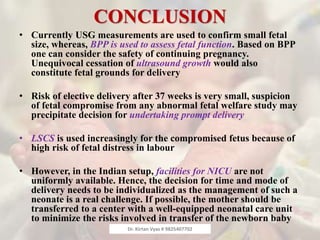
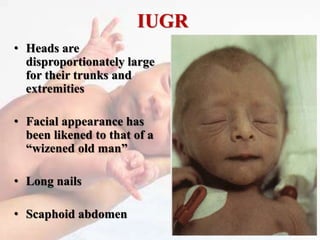
This document provides information from Dr. Kirtan Vyas about fetal growth restriction (FGR). It discusses the challenges in identifying and managing FGR. Key points include:
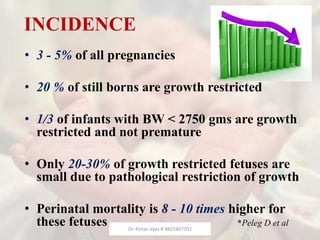
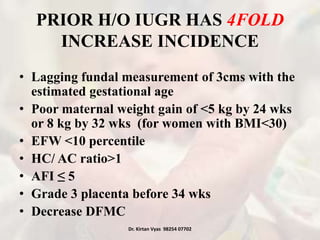
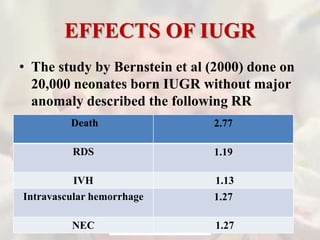
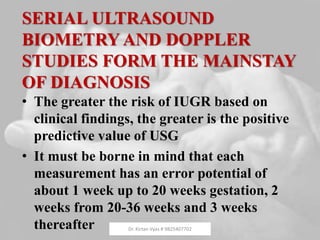
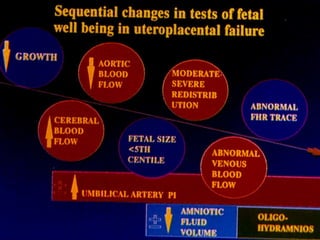
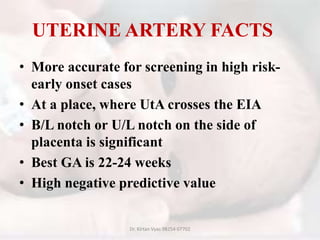
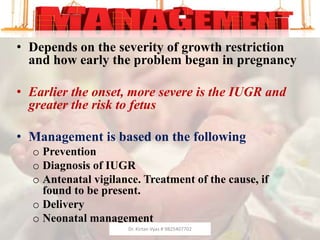
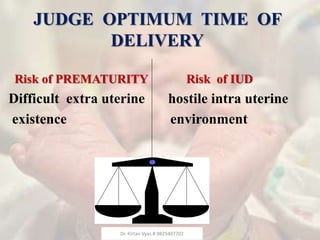
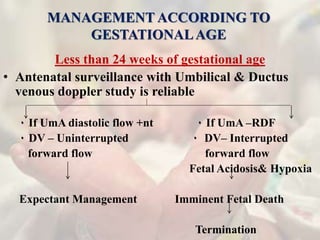
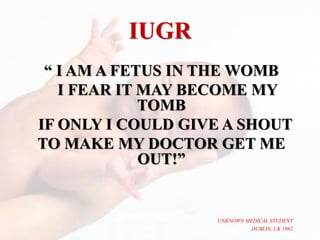
1) Timely identification of FGR is difficult but crucial for proper management and a favorable neonatal outcome, as it is the second leading cause of perinatal mortality after prematurity.
2) FGR remains extensively studied but still confusing and controversial to researchers.
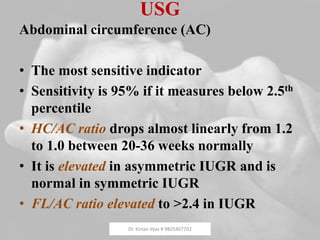
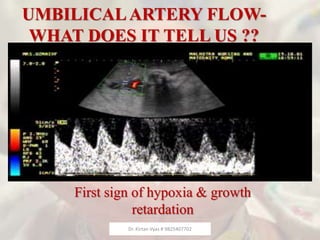
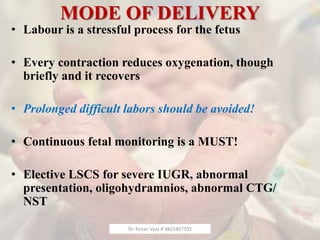
3) The major concern with FGR is not the small size of the fetus but the possibility of life-threatening fetal compromise.
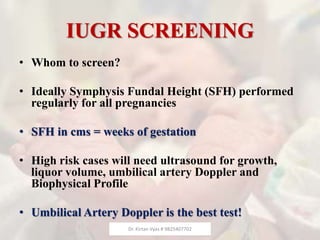
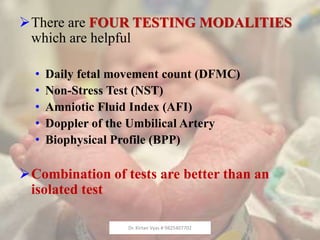
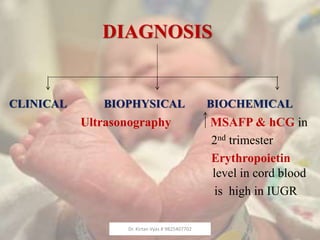
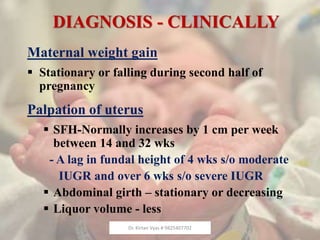
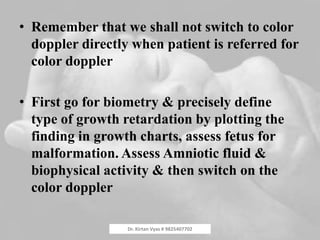
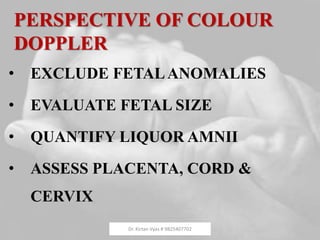
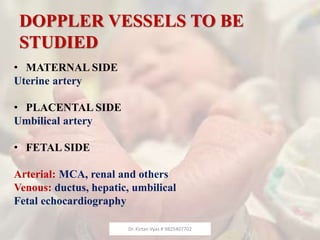
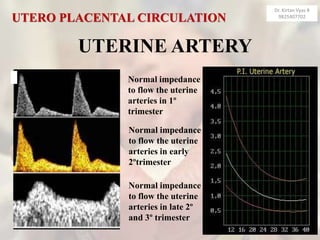
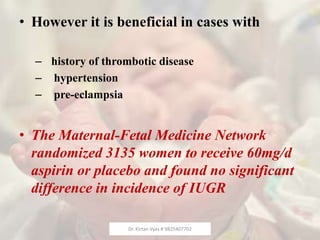
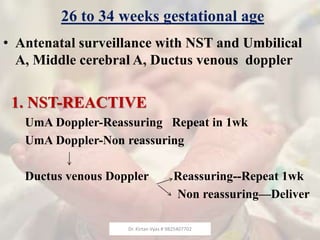
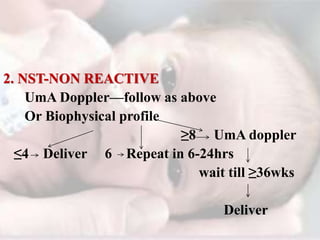
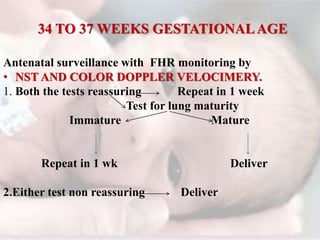
4) Screening approaches, management recommendations, and postnatal care for babies with FGR are discussed.