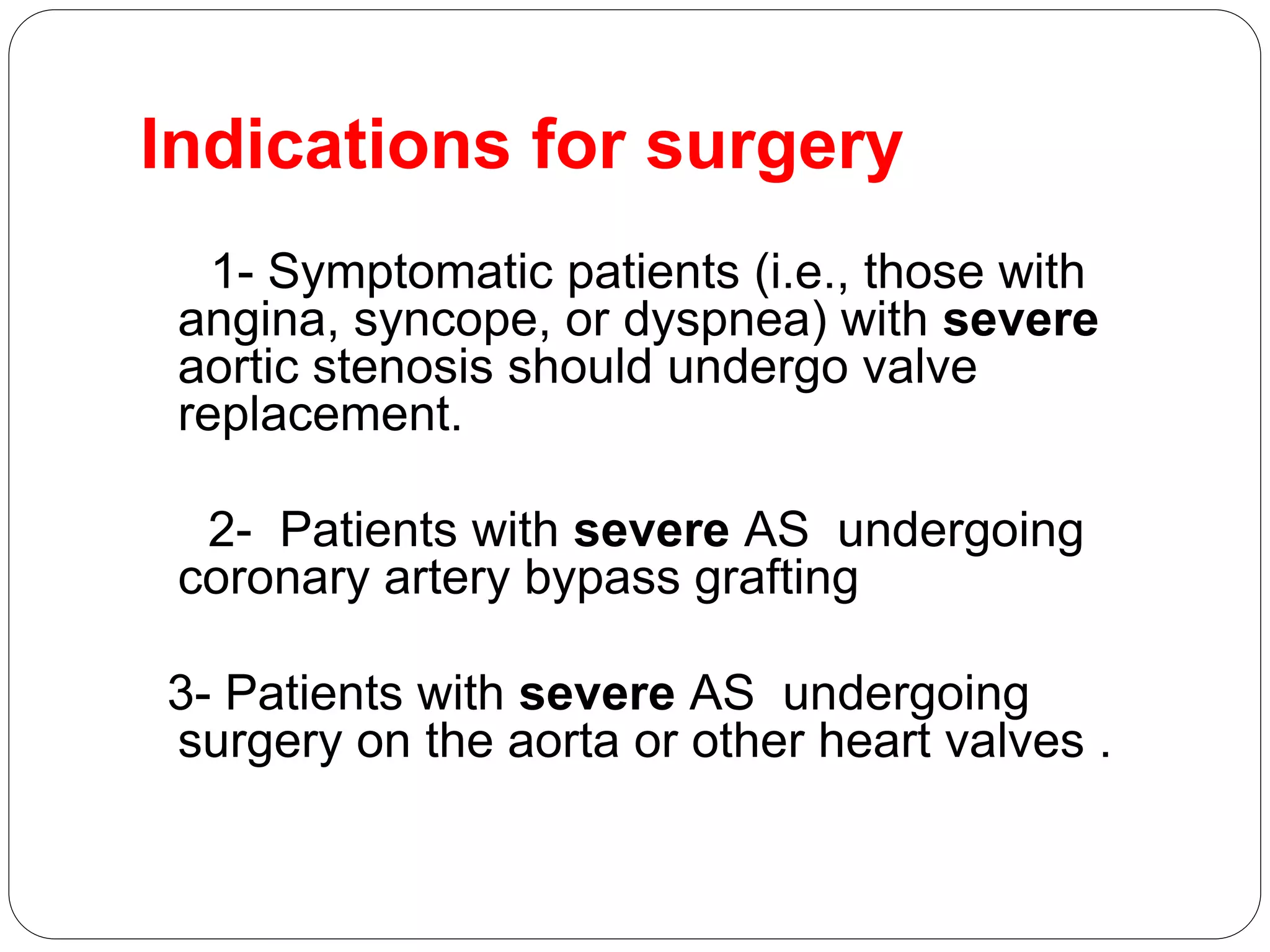
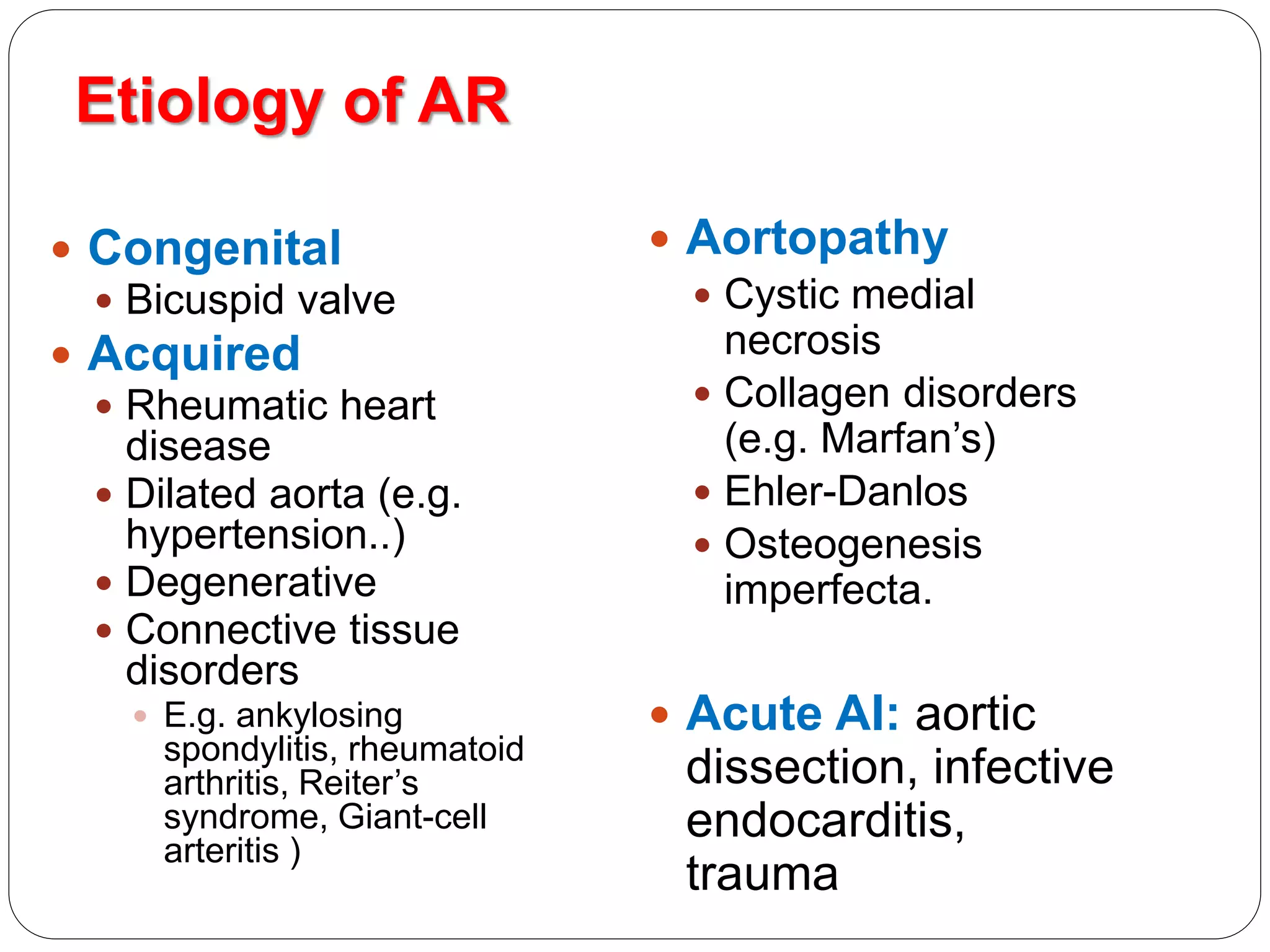
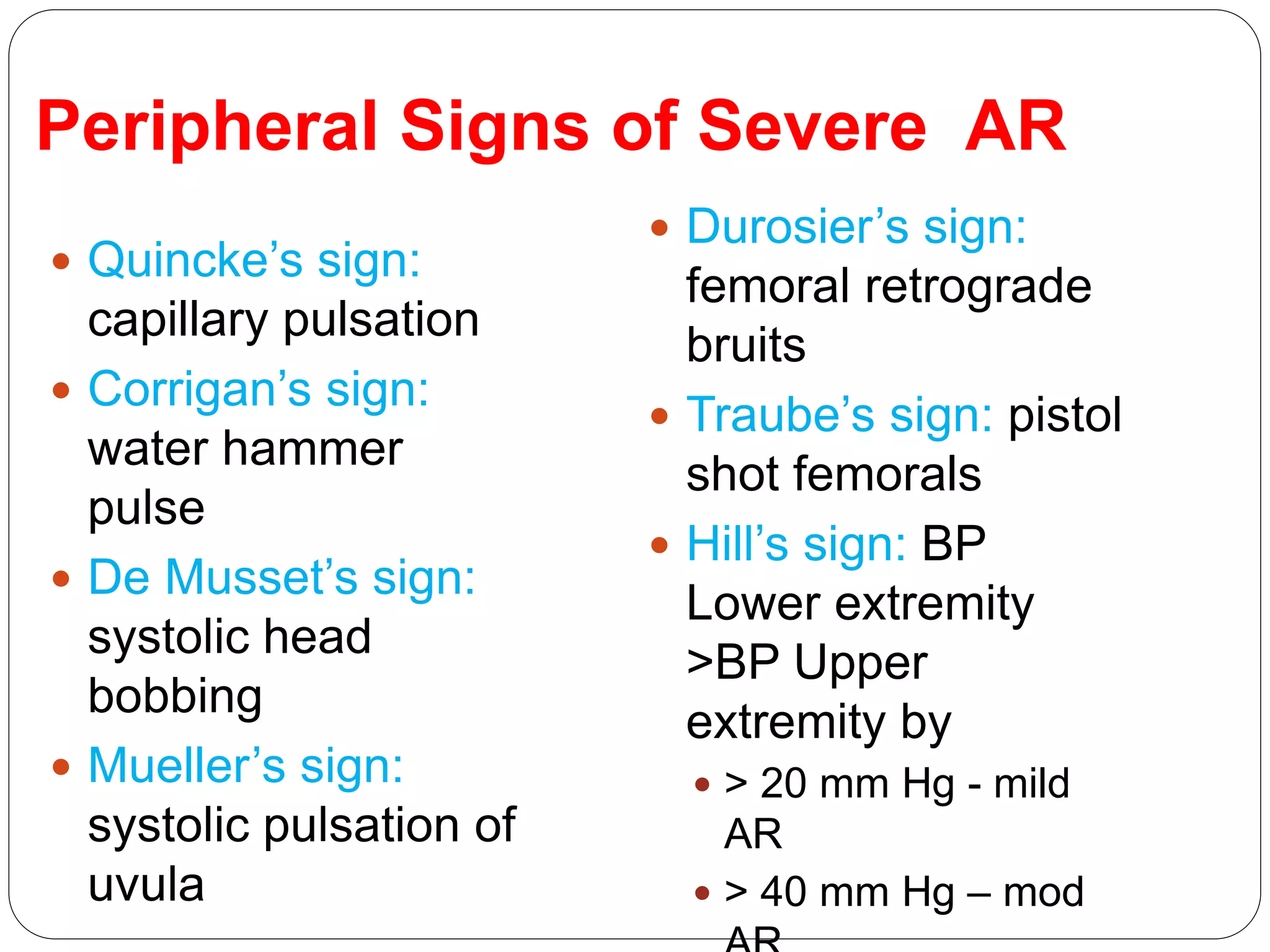
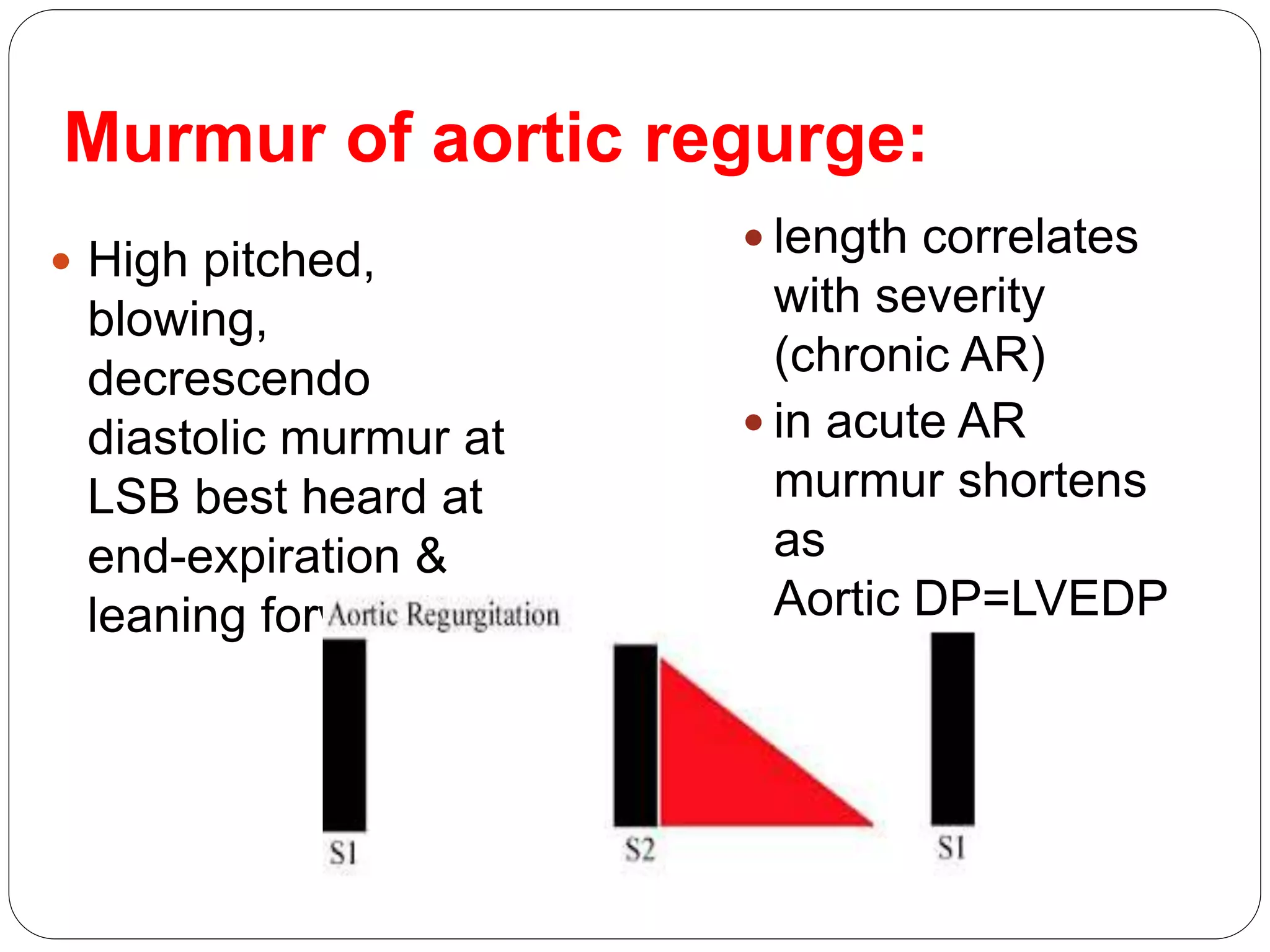
This document discusses aortic valve disease, including aortic stenosis and aortic regurgitation. It provides definitions and descriptions of aortic valve stenosis in terms of etiology, pathophysiology, clinical presentation, investigations, and treatment options including surgical aortic valve replacement and percutaneous approaches. For aortic regurgitation, it covers etiology, pathophysiology, symptoms, physical exam findings for assessing severity, investigations, and indications for surgical valve replacement. Key points are made about compensatory changes in the left ventricle and how these relate to severity and timing of intervention.