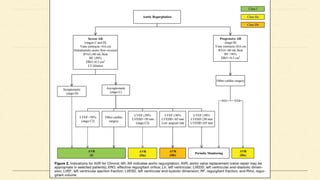
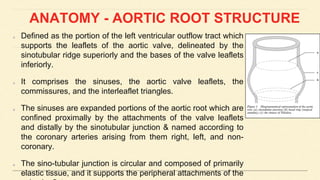
The document provides an in-depth overview of the anatomy and function of the aortic valve and aortic root, detailing its components, physiological roles, and the impact of aortic stenosis and regurgitation on the cardiovascular system. It discusses clinical manifestations, examination findings, diagnostic evaluations, and management strategies for various aortic valve conditions, including echocardiographic assessment parameters for severity. Key points include the relationship between aortic pressure, ventricular function, and the importance of proper measurement techniques in diagnosing aortic valve diseases.





![REG- VOL, REG- FRACTION & ERO
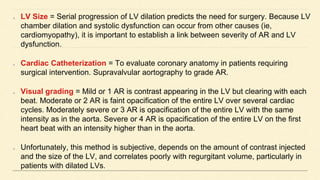
Regurgitant volume is the difference between the systolic flow across the aortic valve and
“net forward” cardiac output.
In the absence of intracardiac shunts and mitral regurgitation, flow through the pulmonary
artery or mitral valve is equivalent to (net) cardiac output. Pulmonary artery blood flow is
reliably measured with TEE by measuring the pulmonary artery diameter (d), calculating
its area [π (d/2)2], and multiplying the area by the pulmonary artery VTI and heart rate.
Aortic valve systolic flow is the product of aortic valve area and VTI.
Regurgitant Volume = Aortic Valve Systolic Flow – Cardiac Output
Regurgitant Fraction = Regurgitant Volume / Aortic Valve Systolic Flow
ERO = AORTIC ROOT area X AORTIC ROOT DIASTOLIC vti / AV Regurgitant JET
vti](https://image.slidesharecdn.com/aorticvalverepairreplacement-240430070705-1cd5091f/85/Aortic-valve-Repair-Replacement-TEEpptx-50-320.jpg)