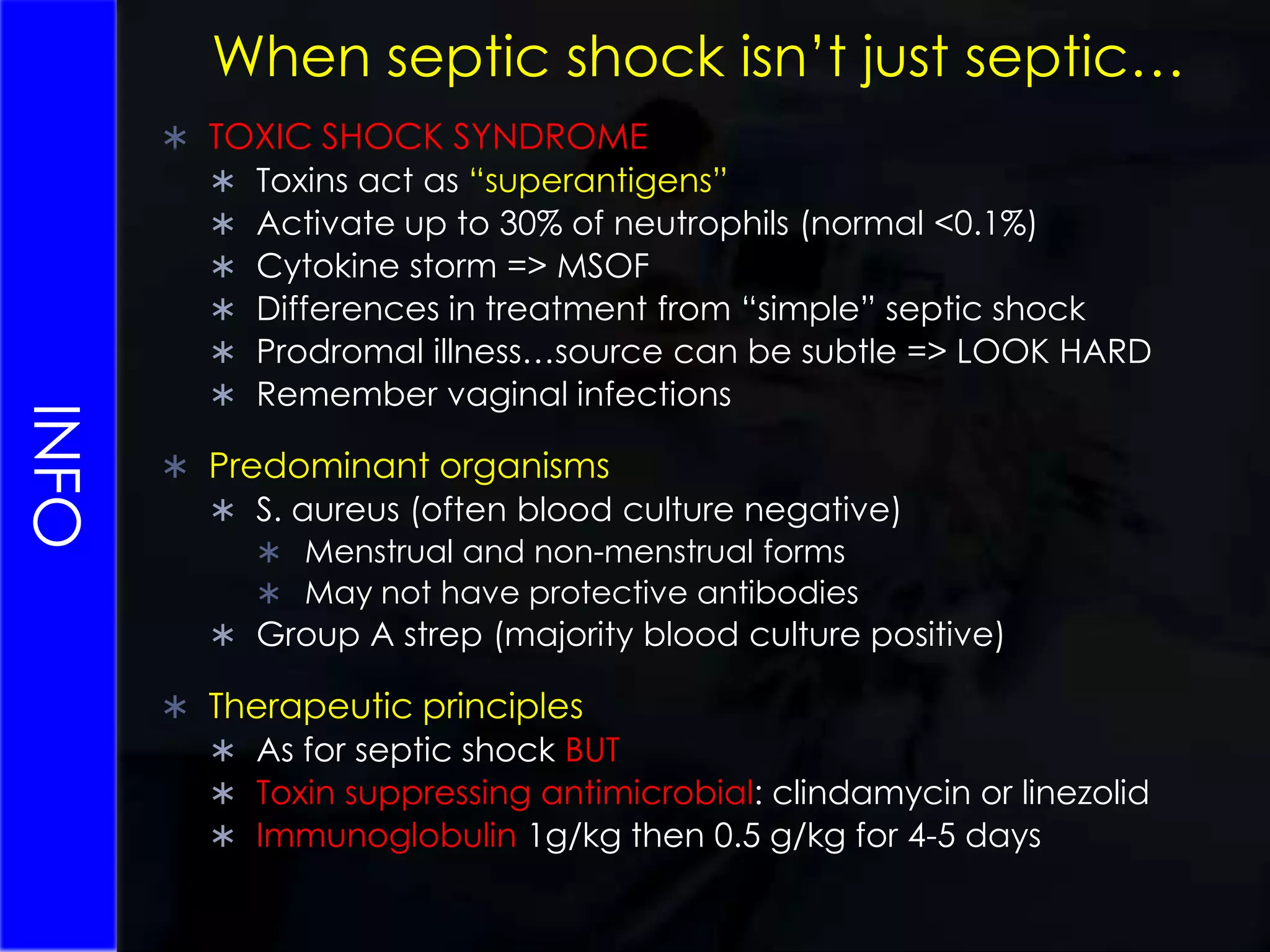
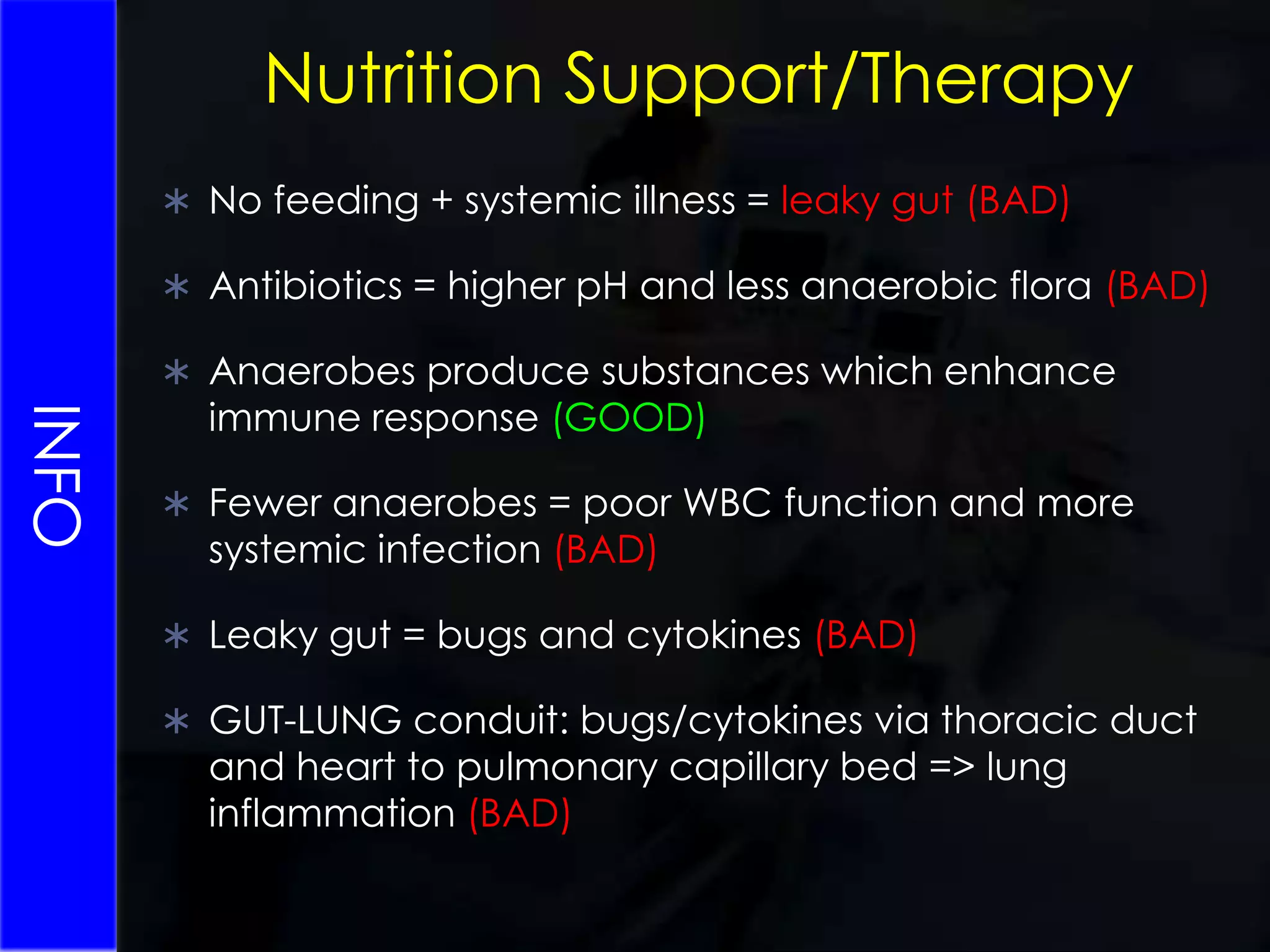
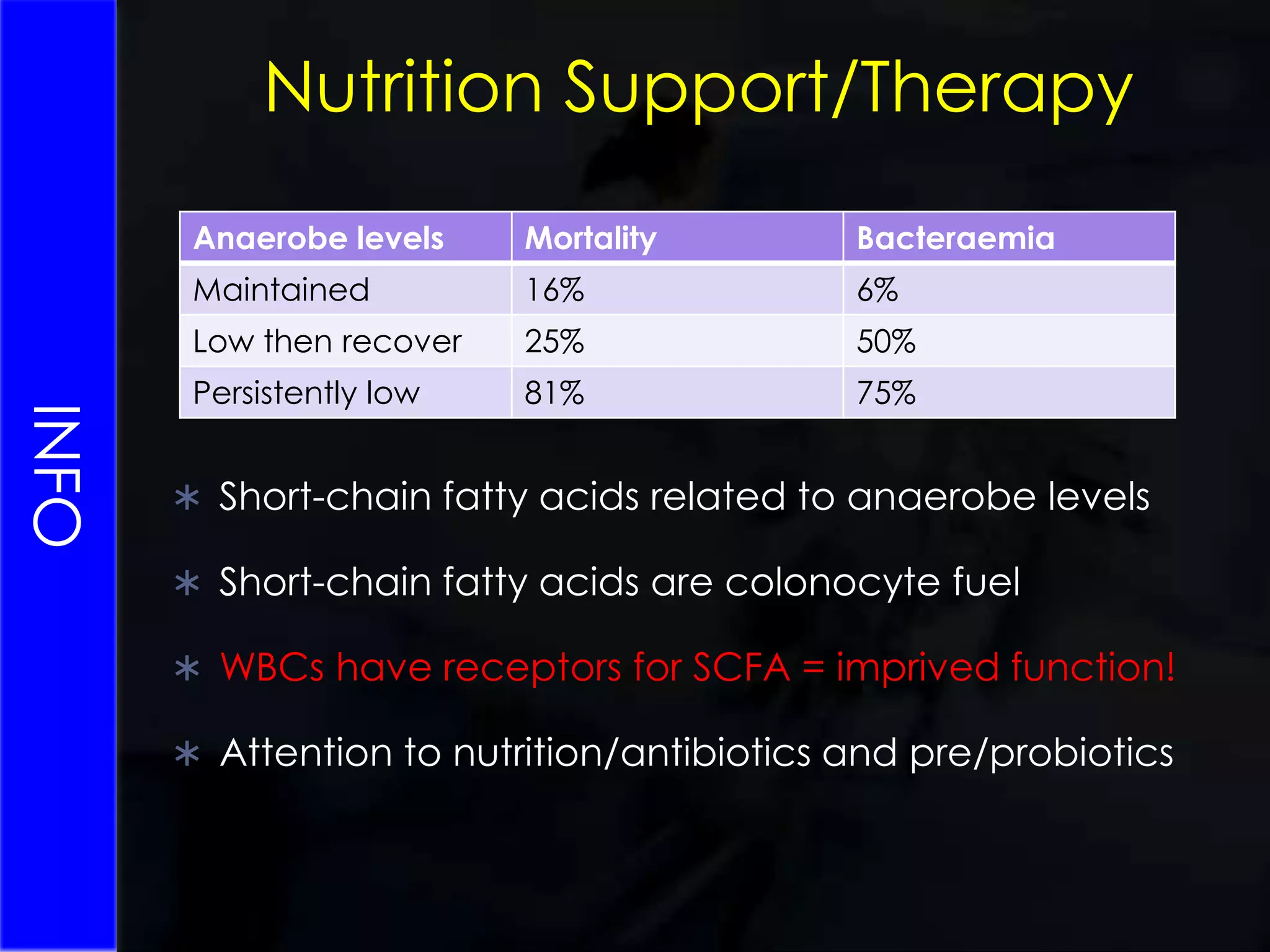
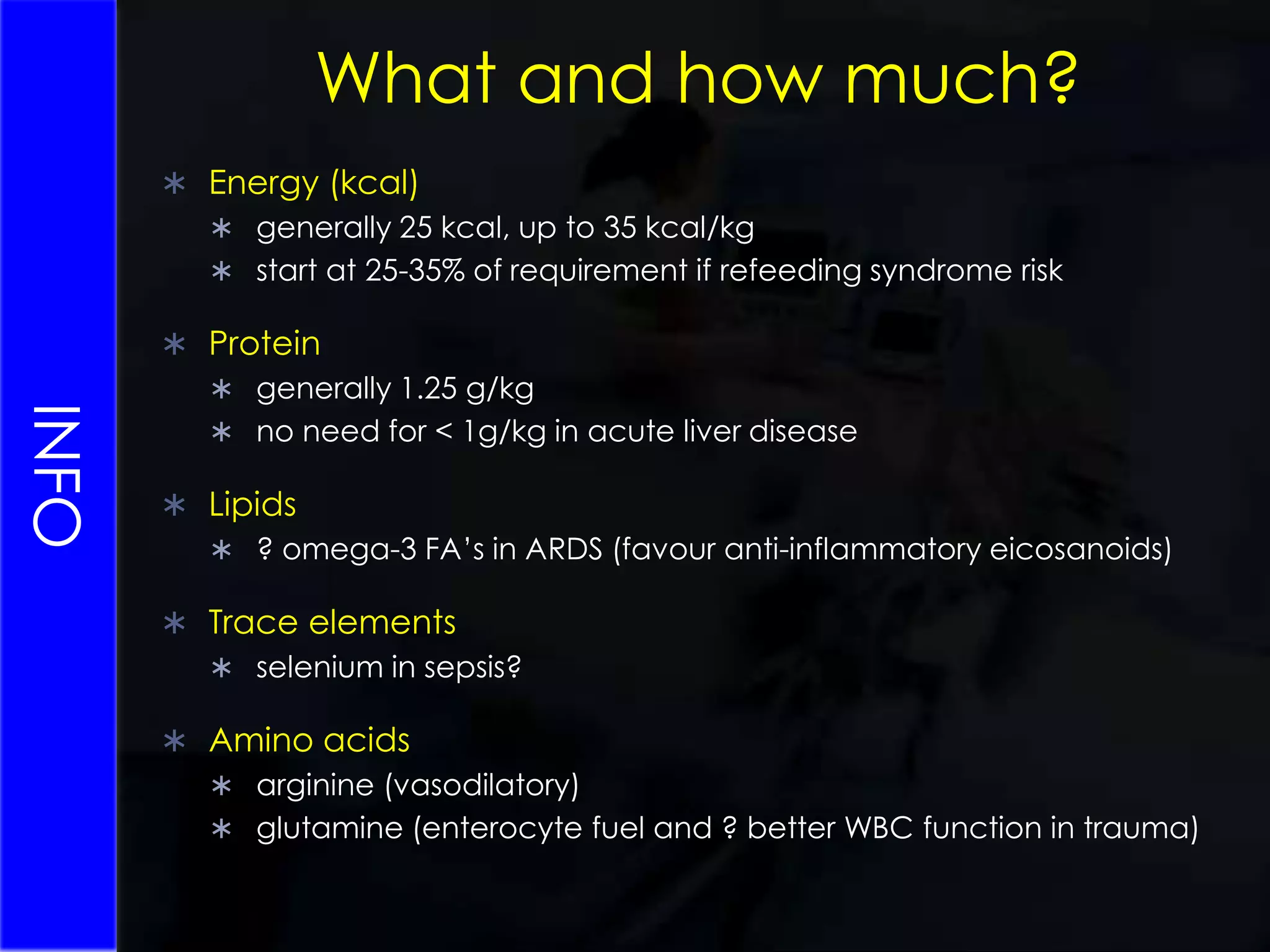
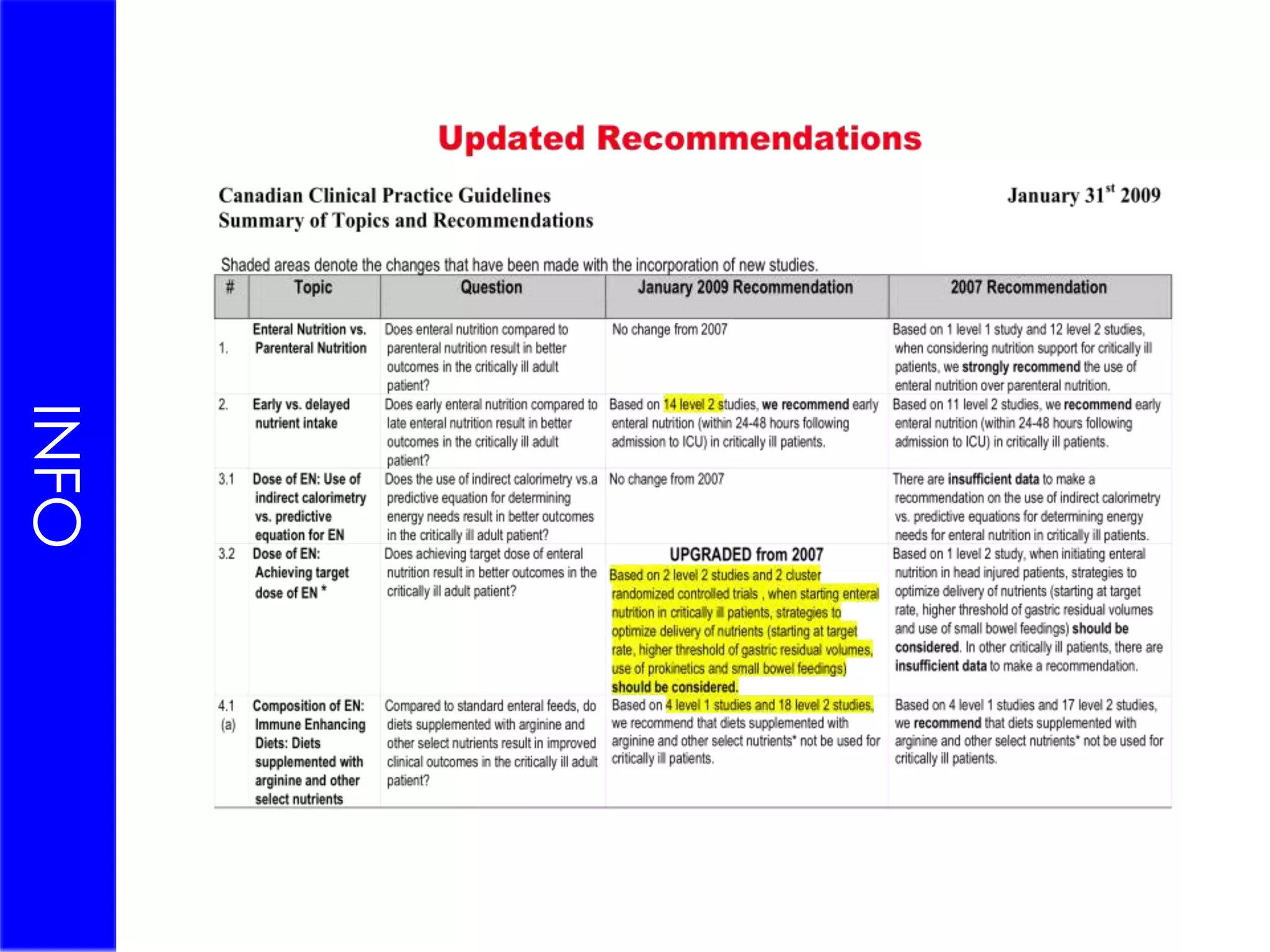
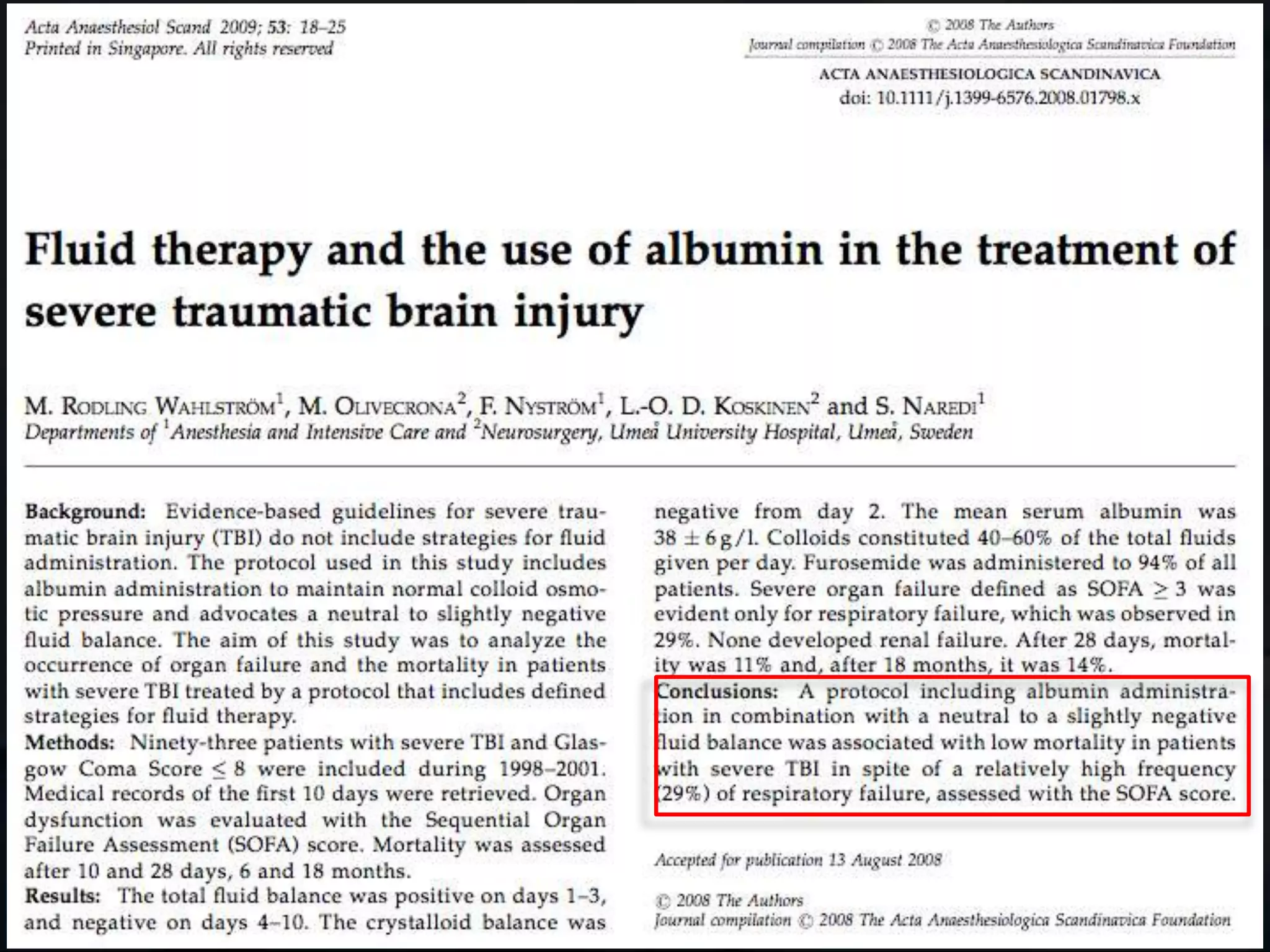
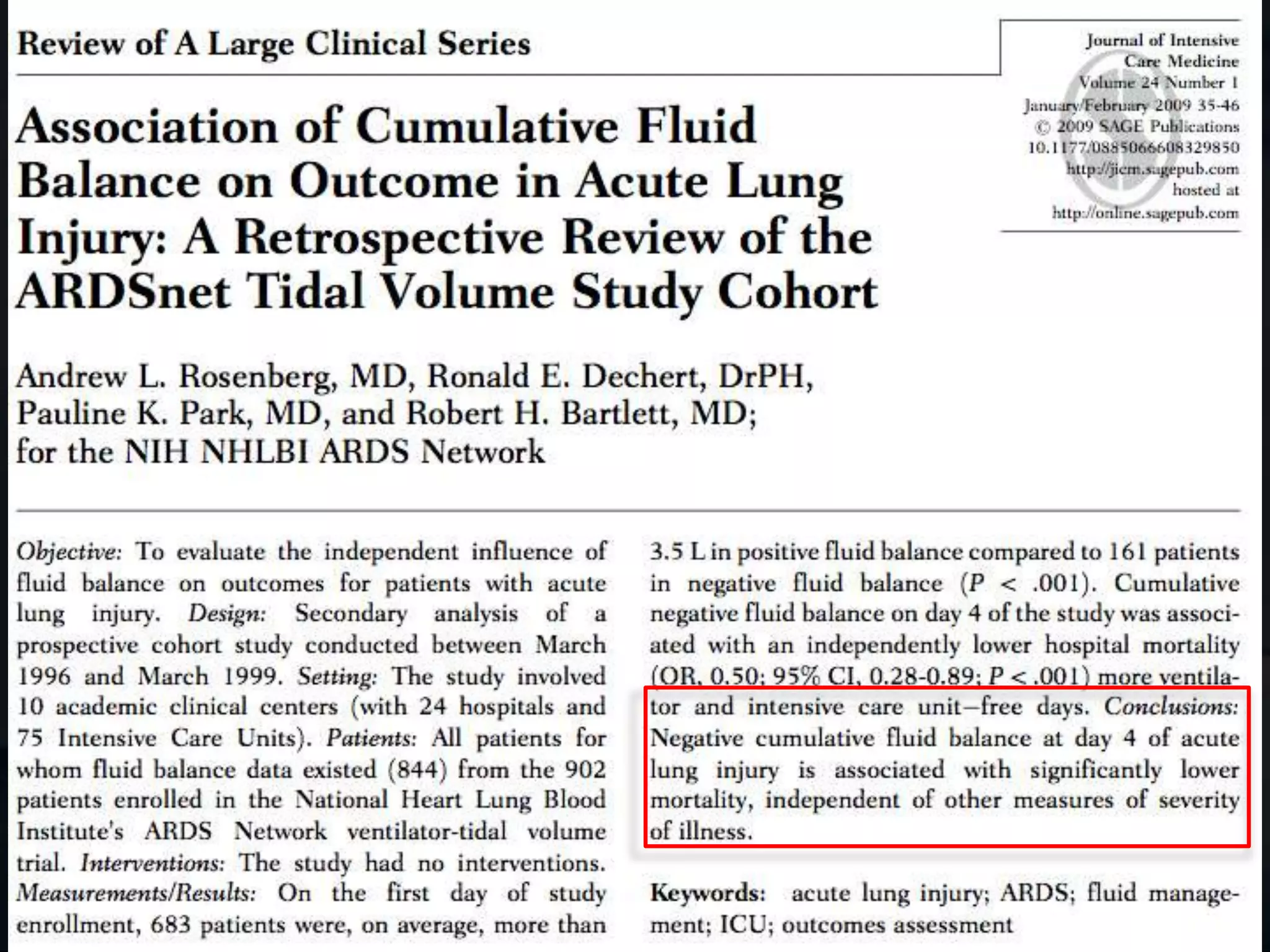
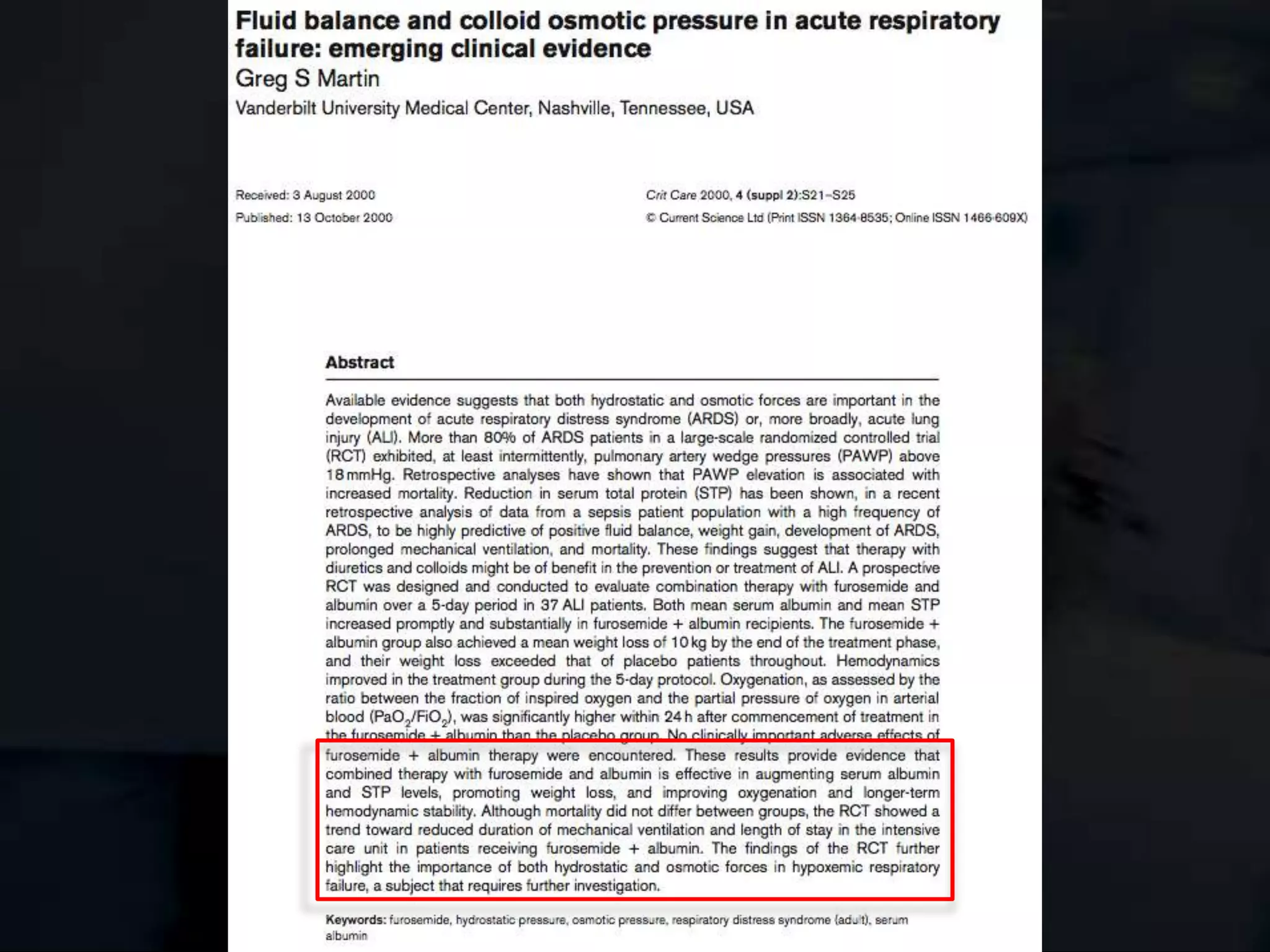
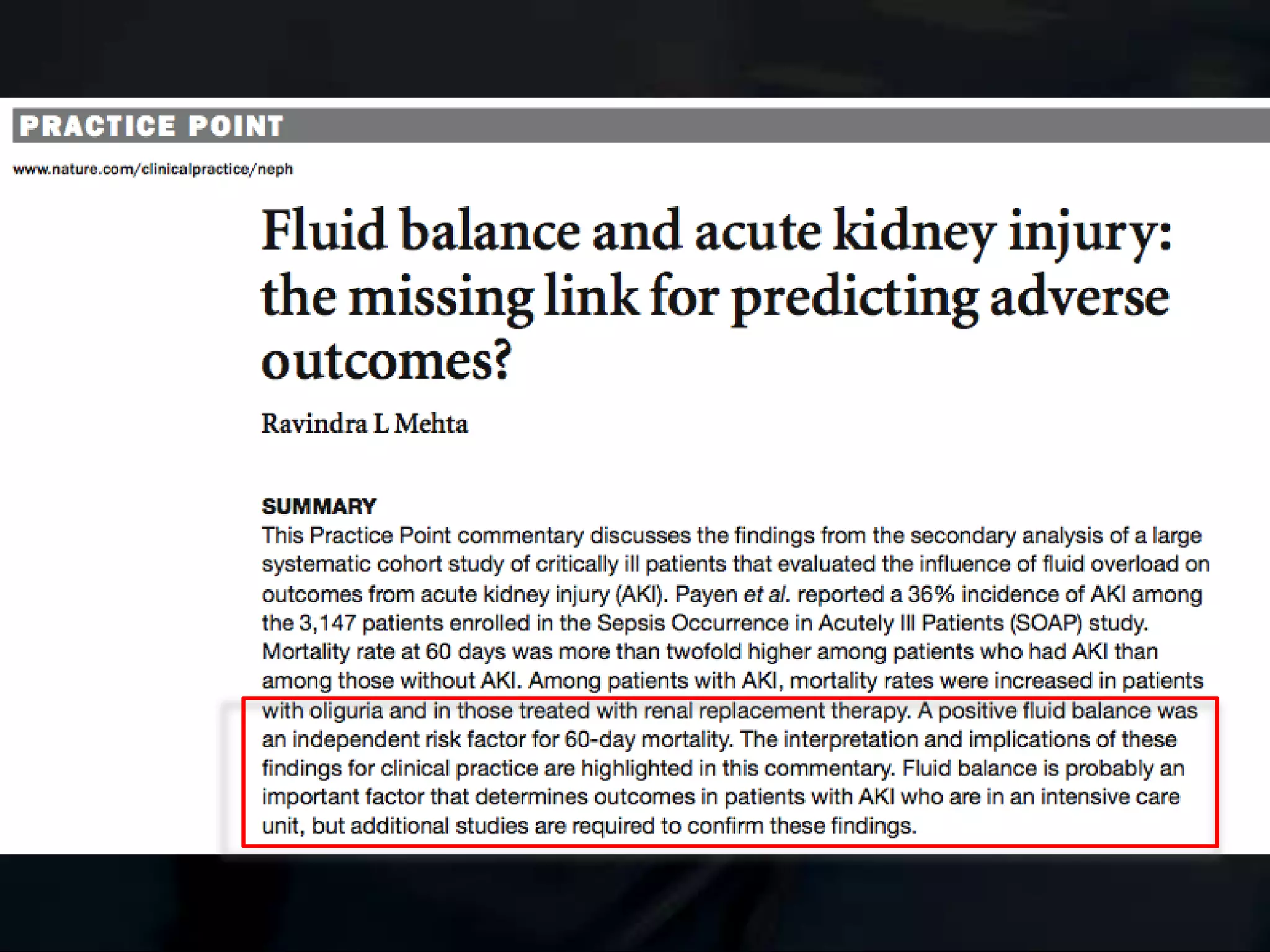
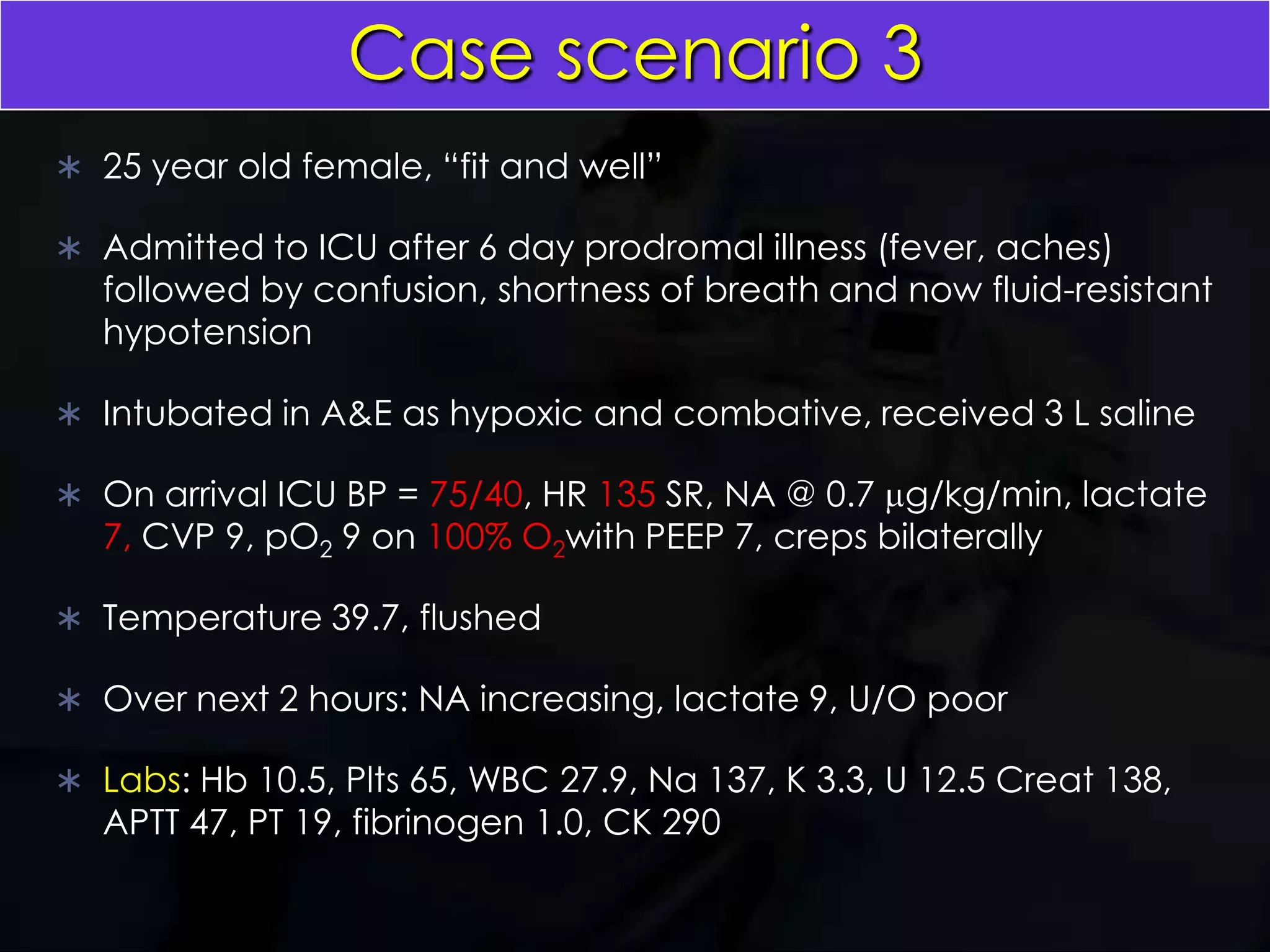
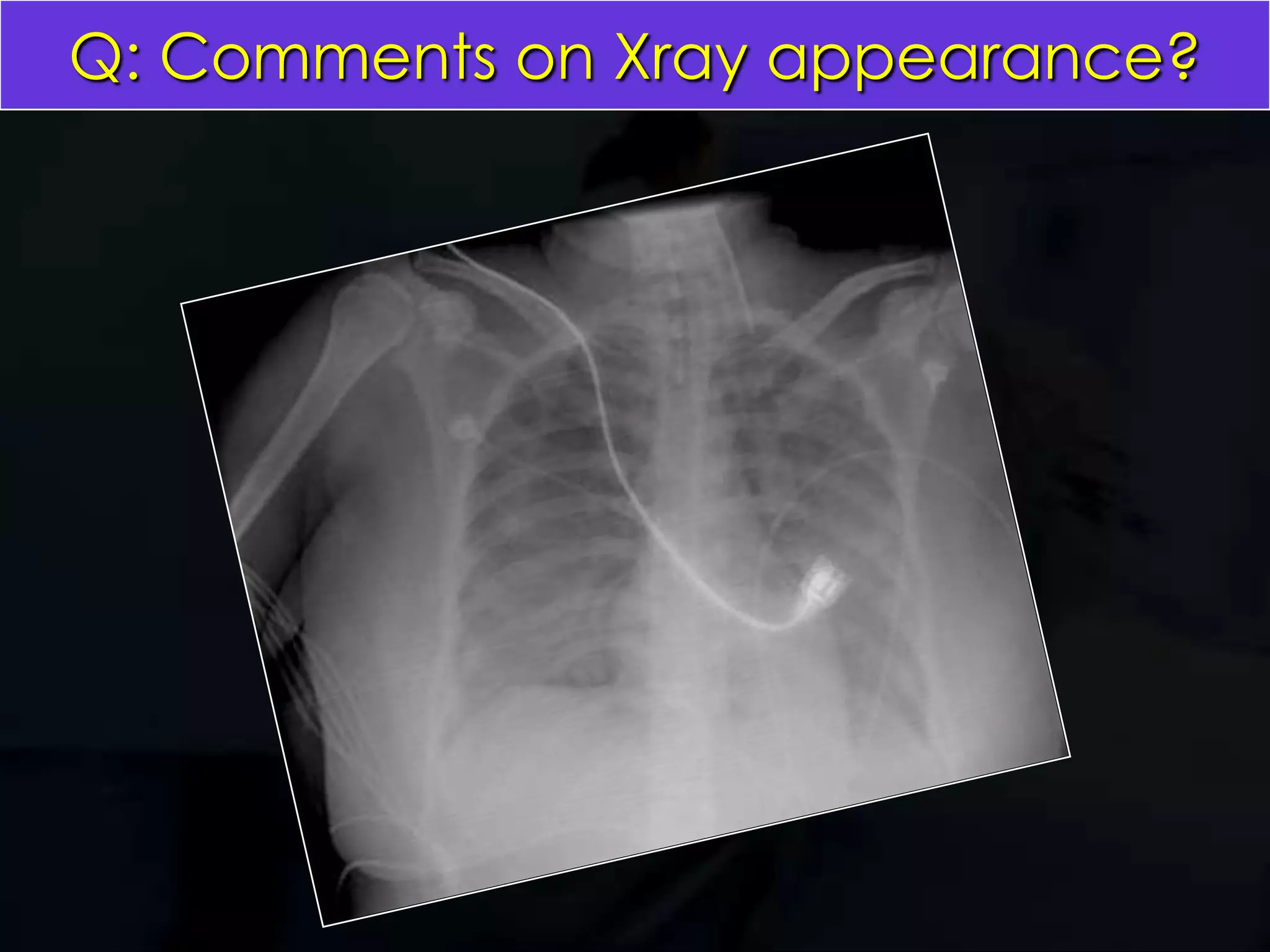
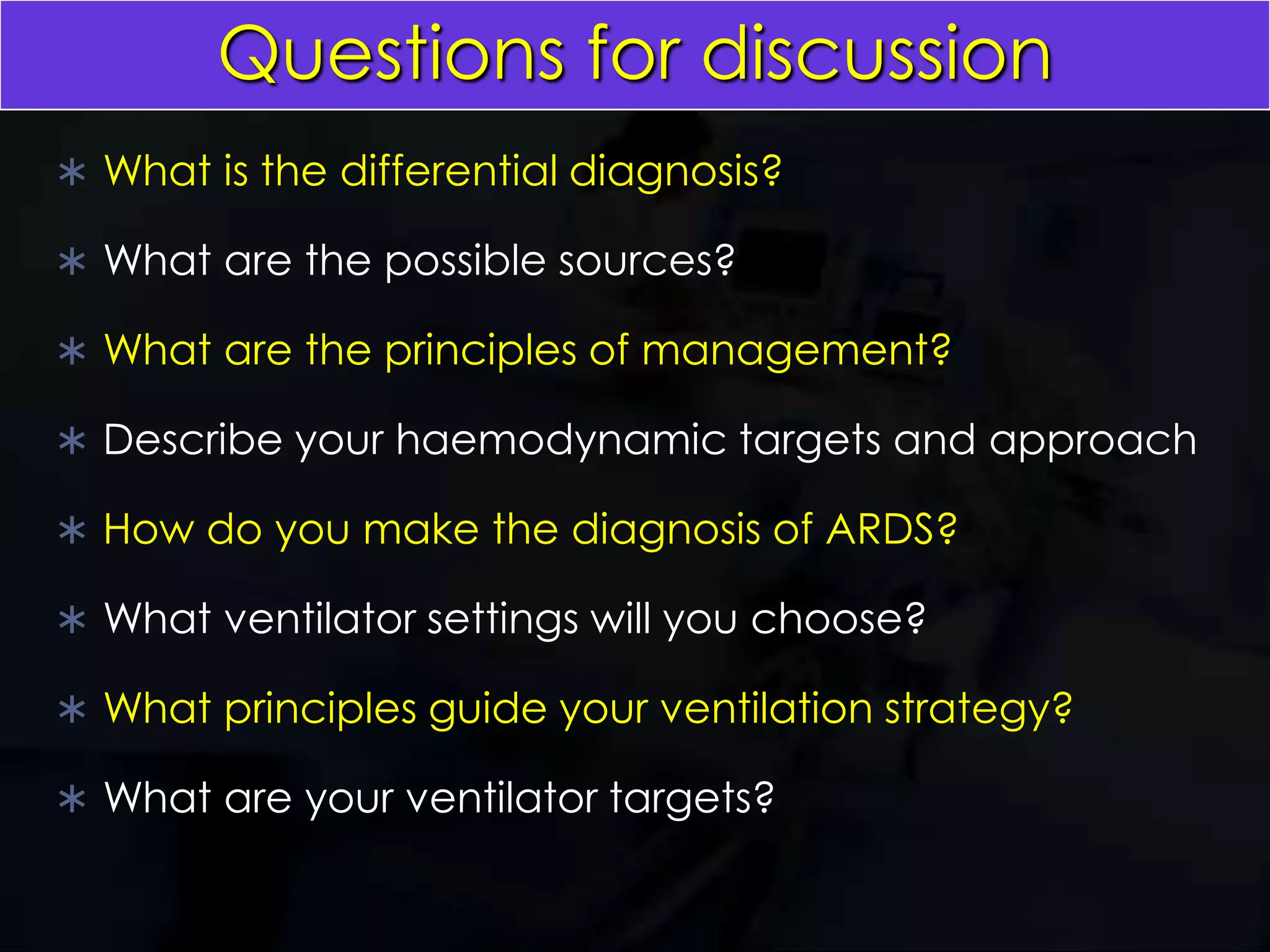
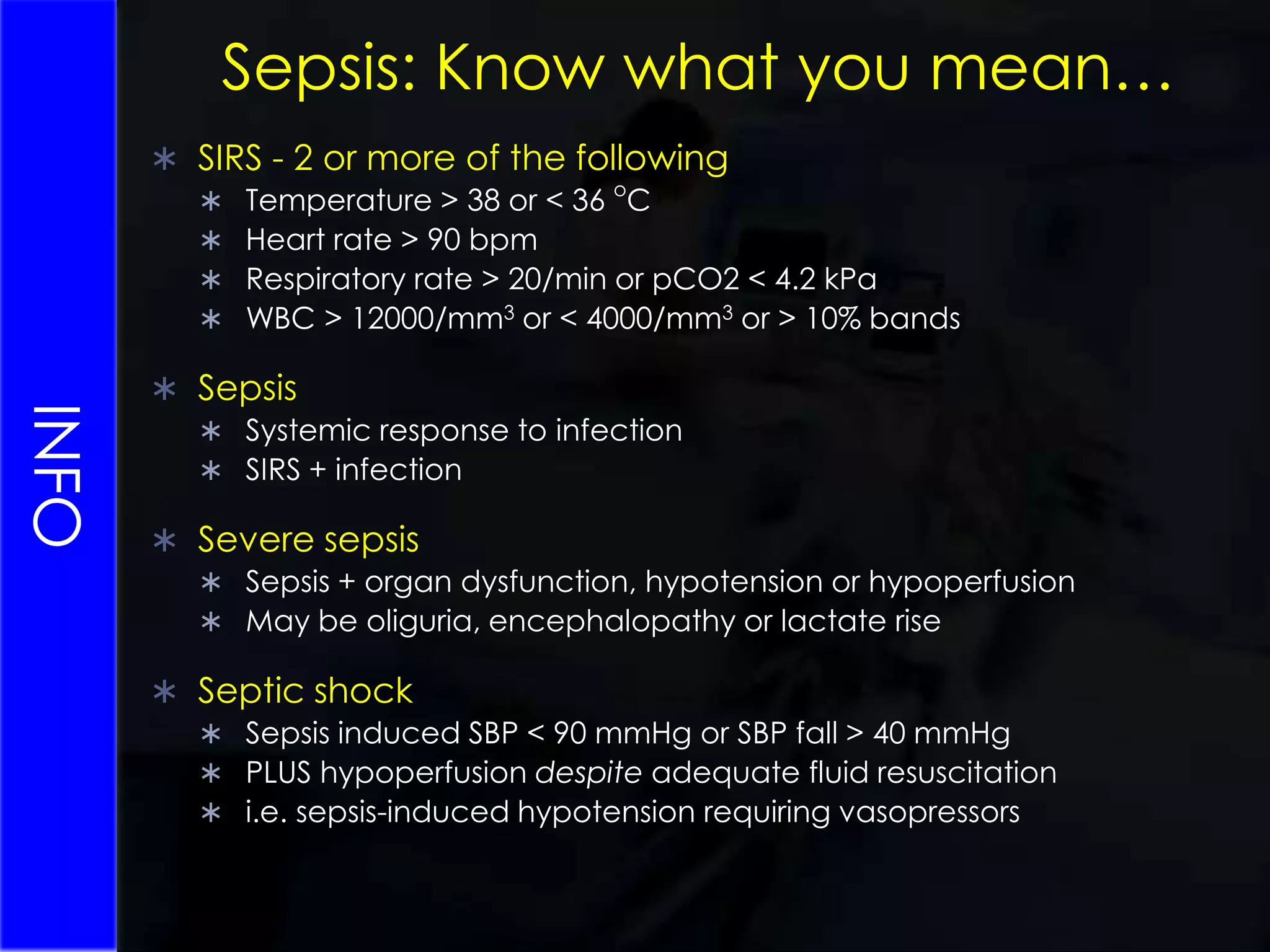
This patient is a 25 year old female admitted to the ICU for respiratory failure and hypotension following a 6 day prodromal illness. She is intubated and receiving vasopressors. The differential diagnosis includes sepsis, severe sepsis, or septic shock from an unknown source. Principles of management include identifying the source, administering appropriate antibiotics, optimizing hemodynamics and organ function, and providing lung protective ventilation for her acute respiratory distress syndrome. Early enteral nutrition is important to support her systemic immune response and prevent further organ dysfunction from a cumulative energy deficit.
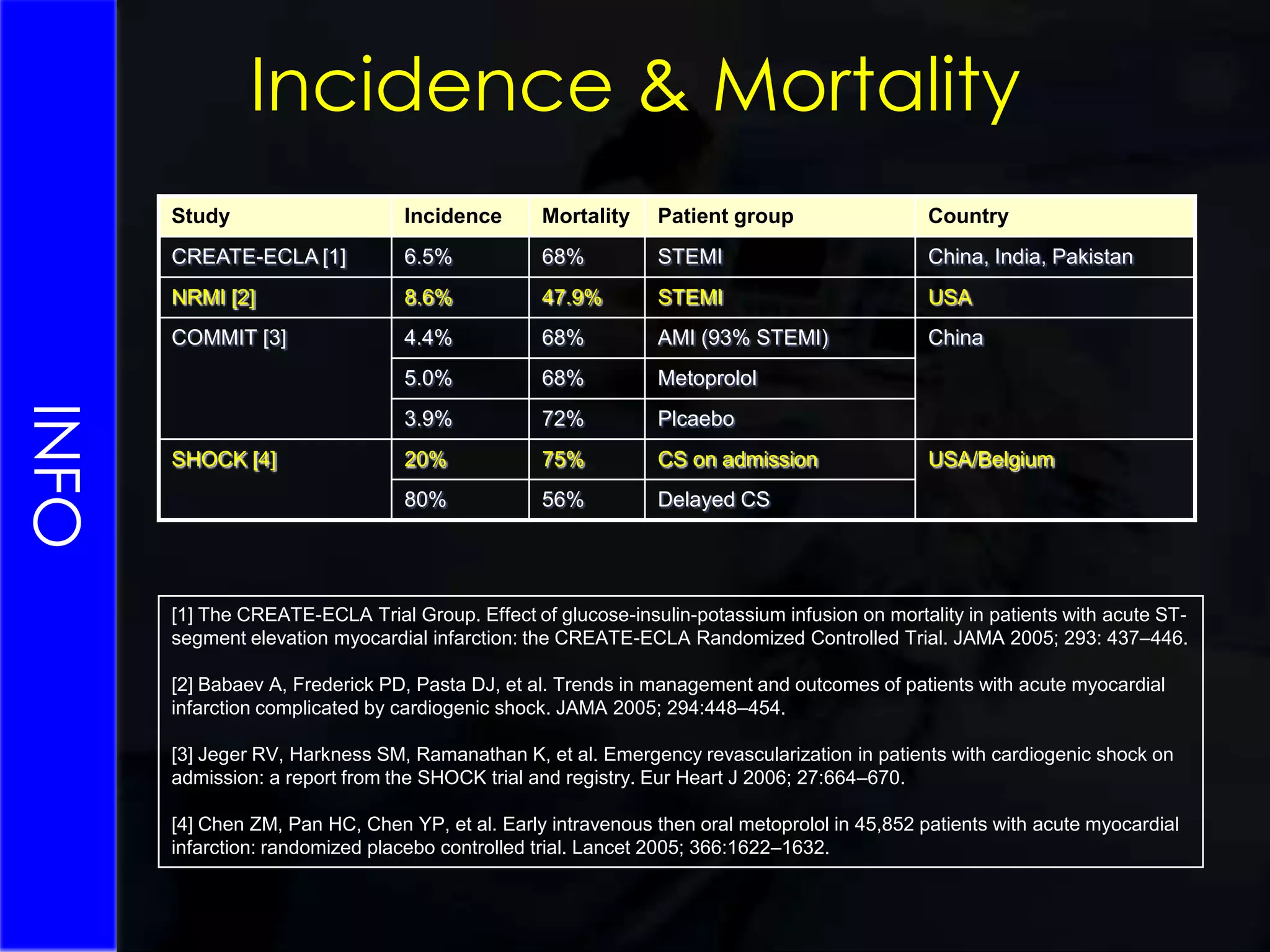
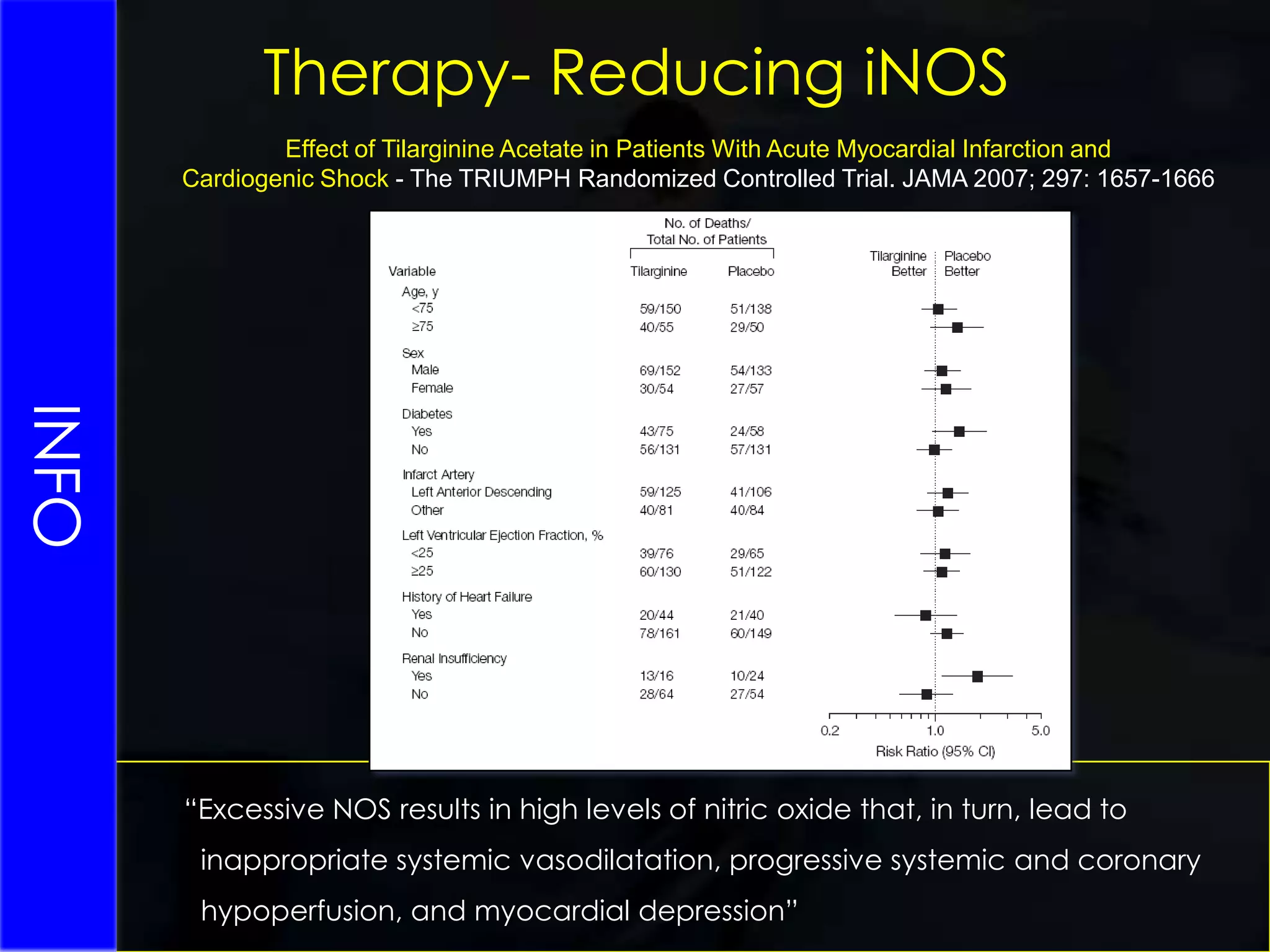
![SVR > 2100 dynes-sec·cm–5INFOIncidence & Mortality[1] The CREATE-ECLA Trial Group. Effect of glucose-insulin-potassium infusion on mortality in patients with acute ST-segment elevation myocardial infarction: the CREATE-ECLA Randomized Controlled Trial. JAMA 2005; 293: 437–446.[2] Babaev A, Frederick PD, Pasta DJ, et al. Trends in management and outcomes of patients with acute myocardial infarction complicated by cardiogenic shock. JAMA 2005; 294:448–454.[3] Jeger RV, Harkness SM, Ramanathan K, et al. Emergency revascularization in patients with cardiogenic shock on admission: a report from the SHOCK trial and registry. Eur Heart J 2006; 27:664–670.[4] Chen ZM, Pan HC, Chen YP, et al. Early intravenous then oral metoprolol in 45,852 patients with acute myocardial infarction: randomized placebo controlled trial. Lancet 2005; 366:1622–1632.](https://image.slidesharecdn.com/icutopicsforfinalfrca-100623131625-phpapp01/75/ICU-topics-for-Final-FRCA-39-2048.jpg)