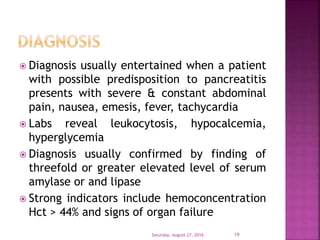
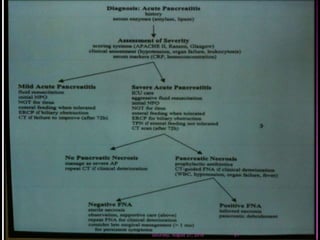
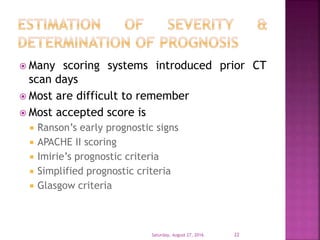
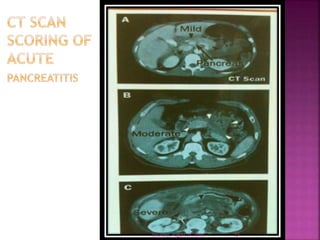
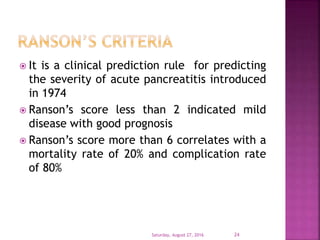
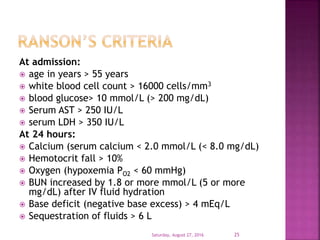
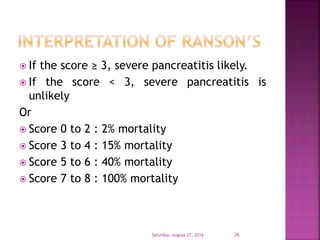
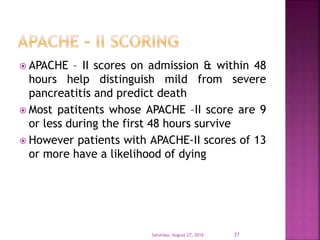
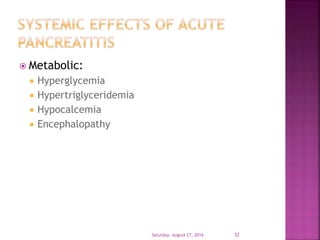
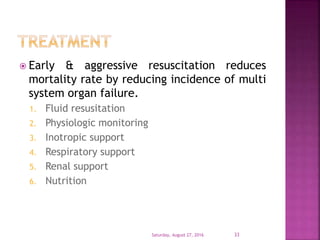
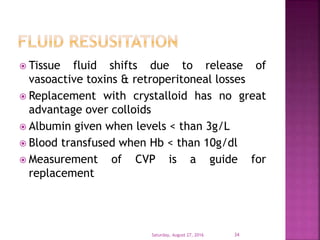
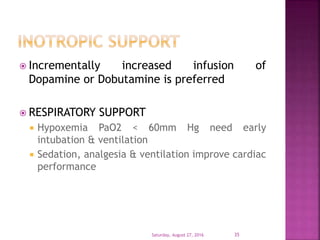
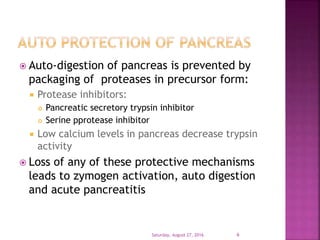
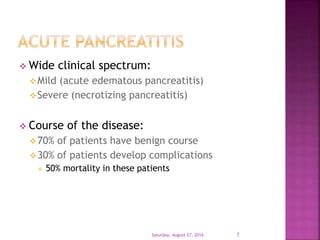
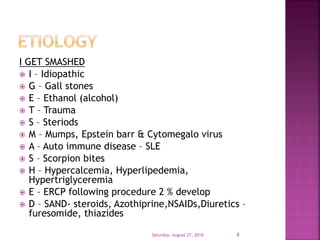
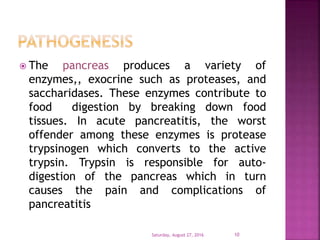
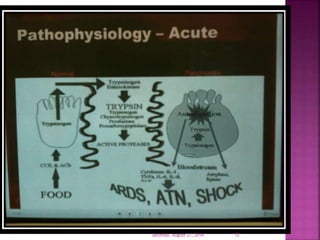
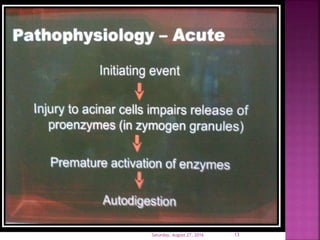
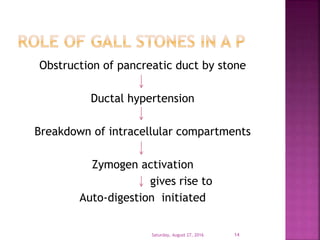
The document discusses acute pancreatitis, highlighting its causes, pathophysiology, and clinical manifestations, including signs and laboratory findings. It elaborates on diagnostic criteria, scoring systems for severity, and management strategies, particularly focusing on the need for early and aggressive resuscitation to reduce mortality. Different complications arising from the condition, as well as nutritional support considerations, are also mentioned.

![ Signs which are less common, and indicate severe disease,
include:
Grey-Turner’s sign(hemorrhagic discoloration of the flanks)
Cullen’s sign (hemorrhagic discoloration of the umbilicus)
Grünwald sign (appearance of ecchymosis around the
umbilicus due to local toxic lesion of the vessels)
Körte's sign (pain or resistance in the zone where the head
of pancreas is located (in epigastrium, 6–7 cm above the
umbilicus)
Kamenchik's sign (pain with pressure under the xiphoid
process)
Mayo-Robson's sign (pain while pressing at the top of the
angle lateral to the erector spinae muscles and below the
left 12th rib (left costo-vertebral angle (CVA))[2]
Saturday, August 27, 2016 15](https://image.slidesharecdn.com/acutepancreatitis-160827202649/85/Acute-pancreatitis-15-320.jpg)