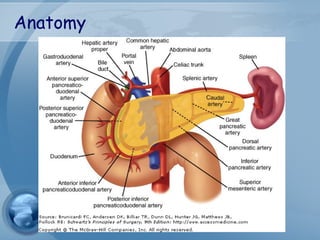
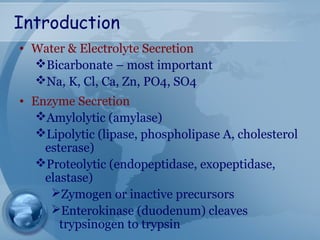
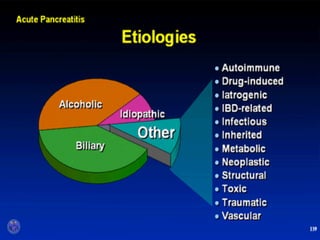
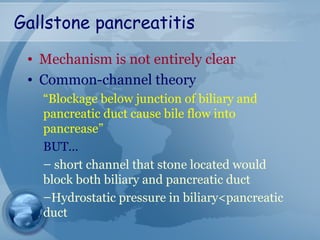
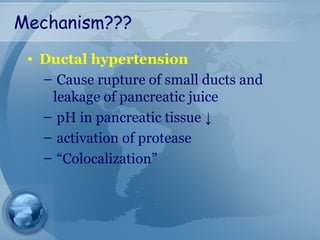
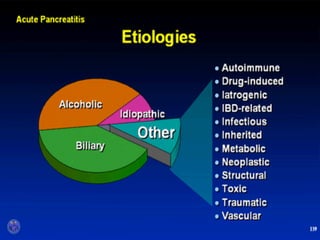
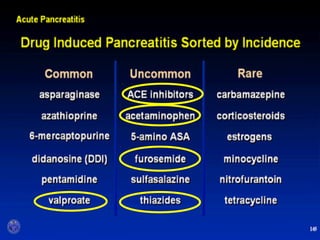
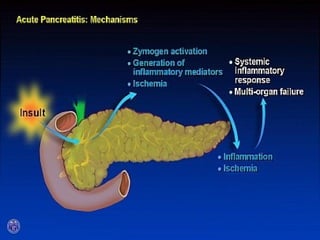
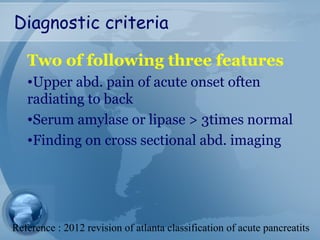
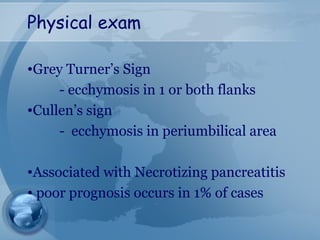
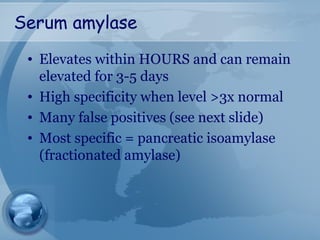
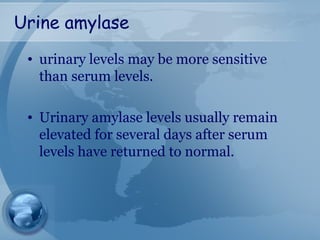
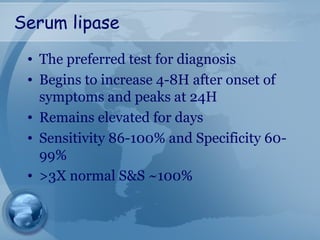
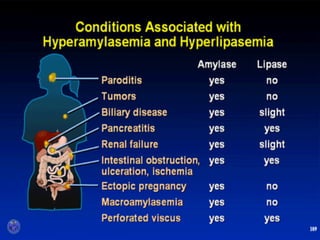
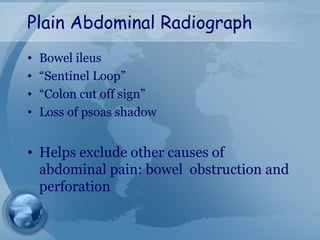
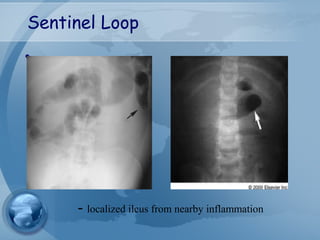
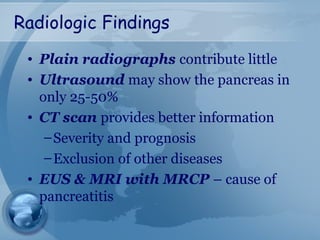
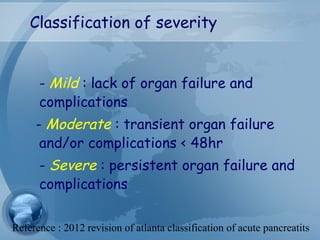
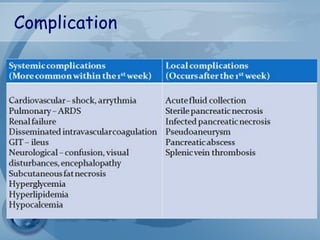
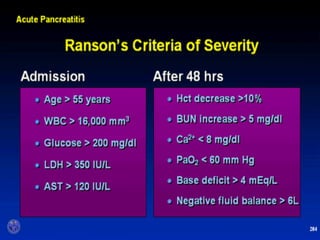
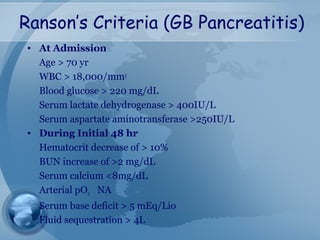
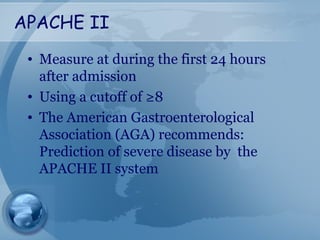
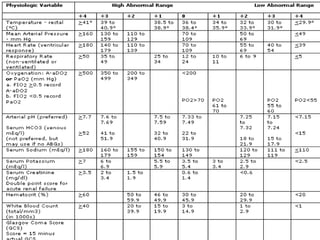
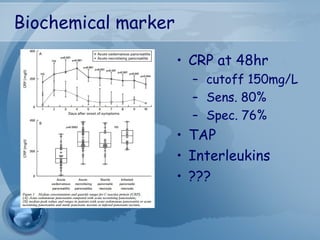
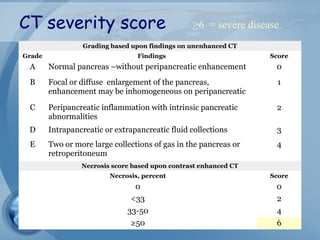
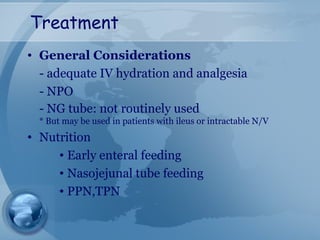
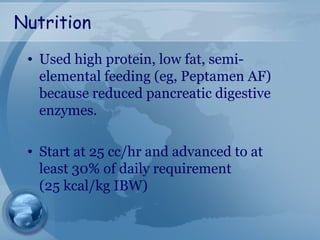
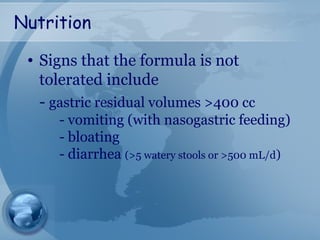
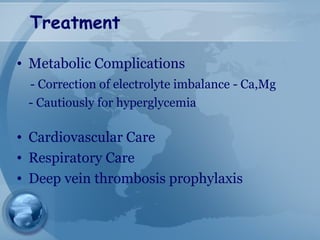
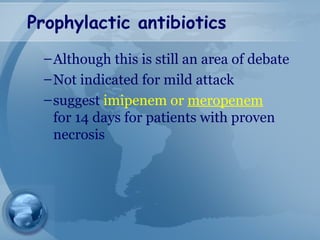
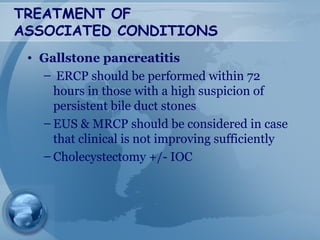
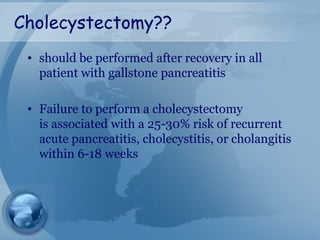
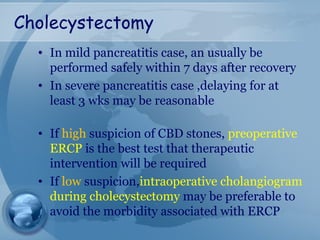
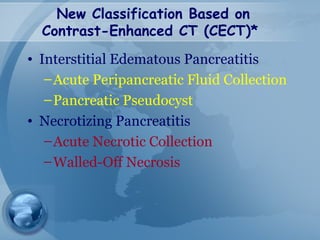
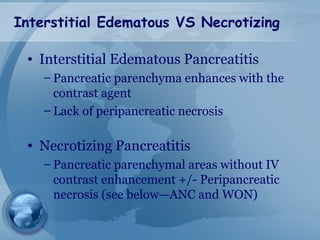
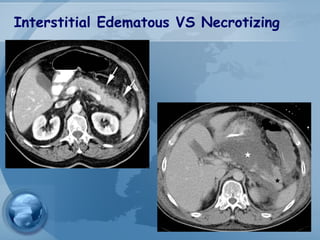
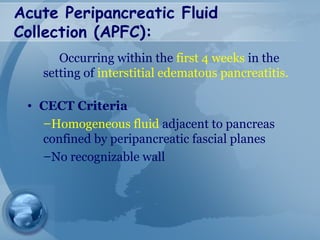
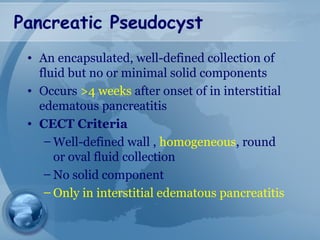
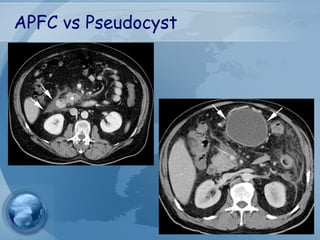
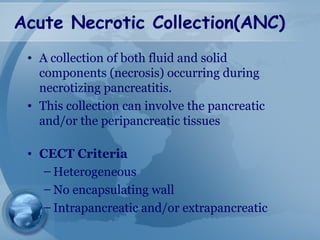
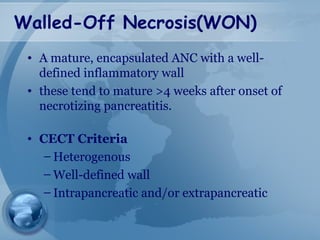
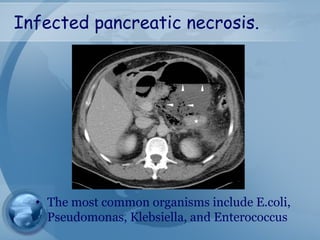
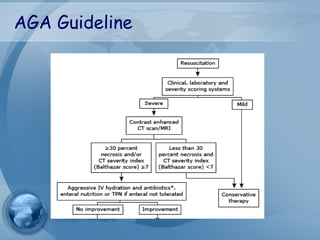
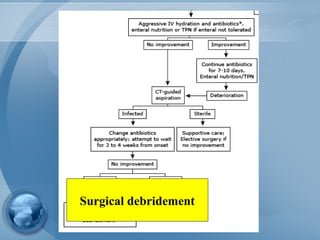
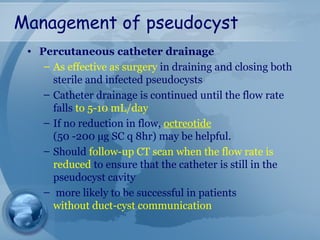
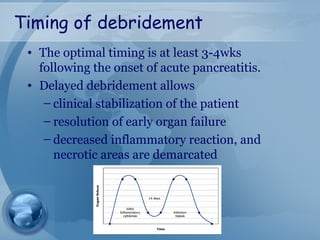
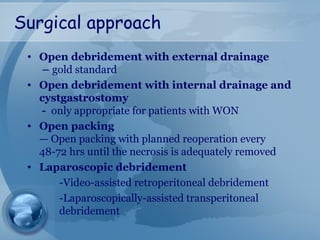
This document discusses acute pancreatitis, including its anatomy, etiology, diagnosis, assessment of severity, treatment, complications, and management guidelines. It covers the key roles of the pancreas in enzyme and electrolyte secretion. Common causes of pancreatitis like gallstones and alcohol are described. Diagnosis involves serum markers, imaging, and severity scores. Treatment focuses on hydration, nutrition, and managing complications. Local complications like pseudocysts and necrosis are defined and approaches to their management are provided. Surgical debridement indications and timing are outlined.