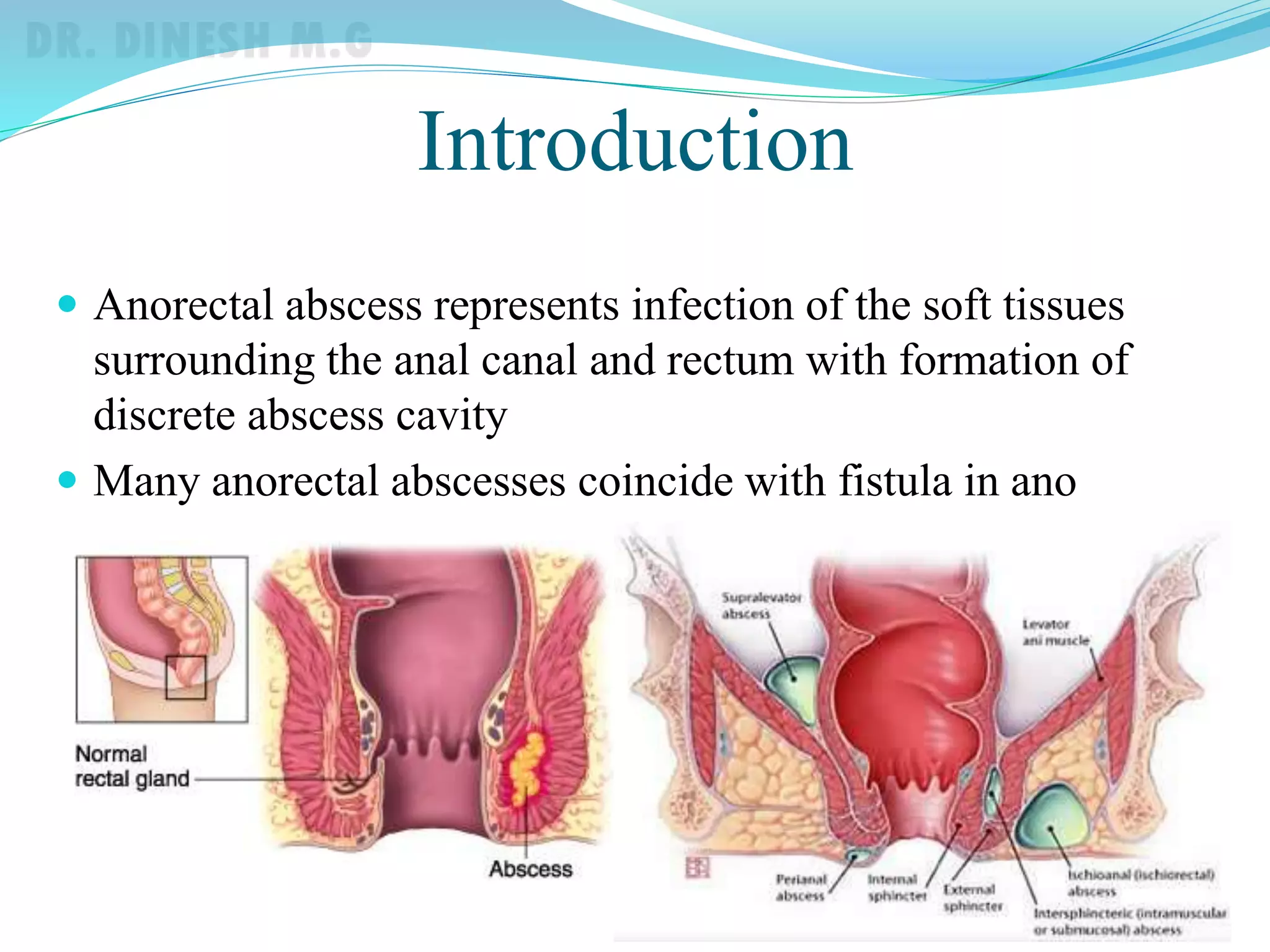
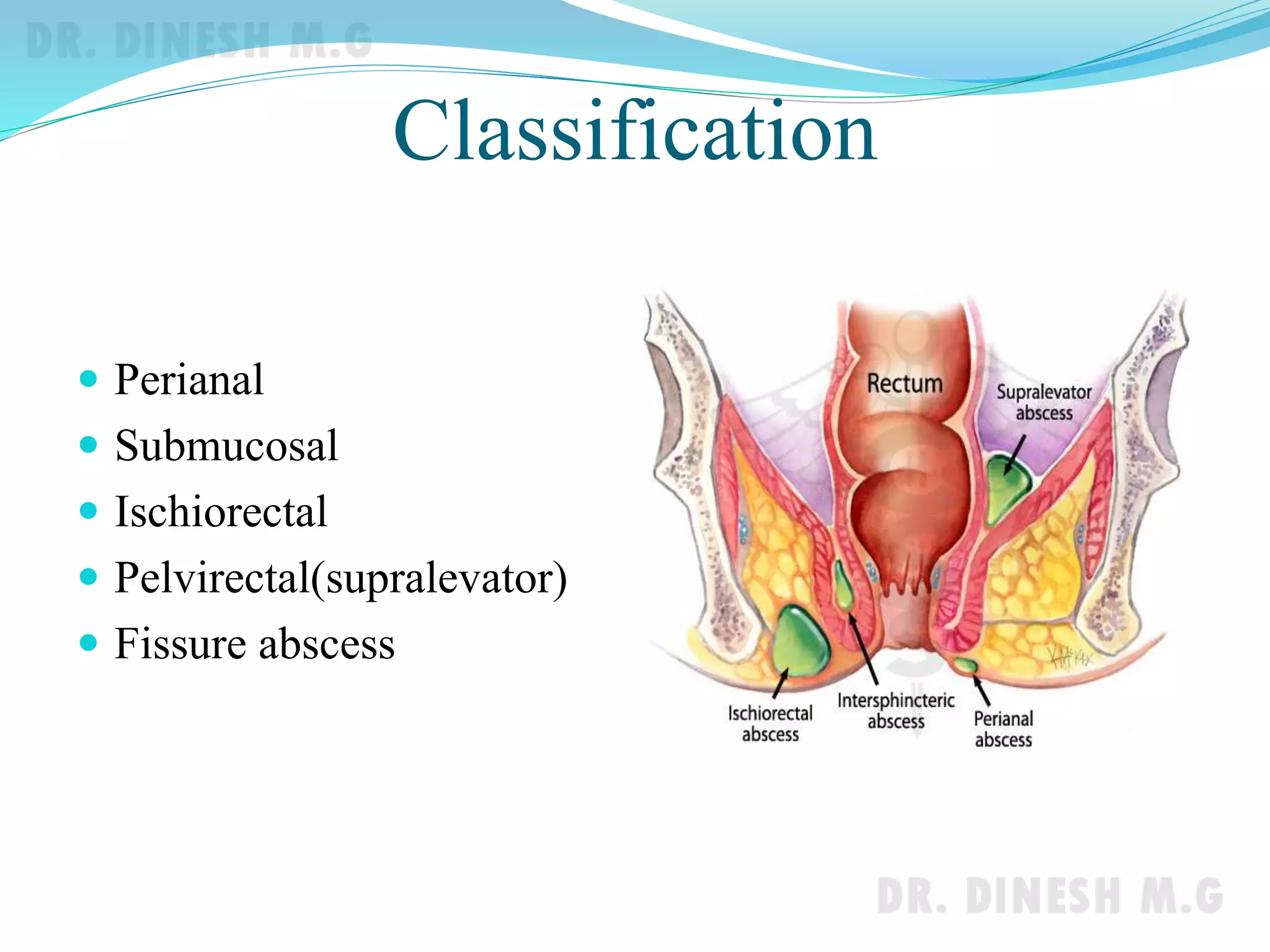
This document discusses anorectal abscesses and fistula in ano. It begins by defining anorectal abscesses as infections of soft tissues around the anal canal that form abscess cavities, often coinciding with fistula in ano. The peak incidence is in the third and fourth decades of life, affecting males more often. Causes include infection of anal glands, injury, Crohn's disease, and tuberculosis. Pathophysiology involves infection of anal glands leading to abscess formation in intersphincteric spaces. Abscesses are classified based on their location such as perianal, ischiorectal, or pelvirectal. Treatment involves incision and drainage. Fistula in ano results from