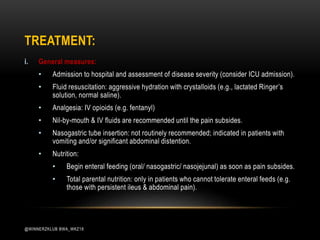
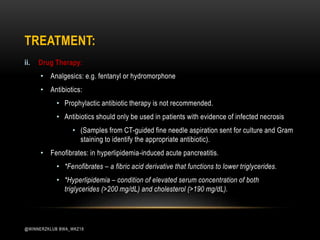
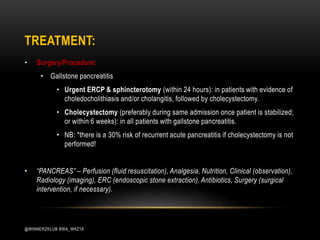
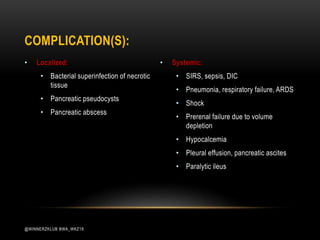
(1) Acute pancreatitis is an inflammatory condition of the pancreas most commonly caused by gallstones or alcohol abuse. (2) Damage to the pancreas leads to release of enzymes that autodigest pancreatic tissue. (3) Treatment involves fluid resuscitation, pain management, monitoring for complications like infection or pseudocyst formation, and identifying and addressing the underlying cause.