Acute pancreatitis.pptx
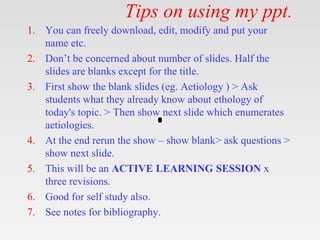
- 1. Tips on using my ppt. 1. You can freely download, edit, modify and put your name etc. 2. Don’t be concerned about number of slides. Half the slides are blanks except for the title. 3. First show the blank slides (eg. Aetiology ) > Ask students what they already know about ethology of today's topic. > Then show next slide which enumerates aetiologies. 4. At the end rerun the show – show blank> ask questions > show next slide. 5. This will be an ACTIVE LEARNING SESSION x three revisions. 6. Good for self study also. 7. See notes for bibliography.
- 3. Learning Objectives 1. Introduction & History 2. Relevant Anatomy, Physiology 3. Aetiology 4. Pathophysiology 5. Pathology 6. Classification 7. Clinical Features 8. Investigations 9. Management 10. Prevention 11. Guidelines 12. Take home messages
- 5. Acute Pancreatitis Definition • Auto digestion of pancreas. • Usually painful and self-limited • Isolated event or a recurring illness • Pancreas returns to normal after (or between) attacks
- 7. Relevant Anatomy and Physiology • neutralize chyme • digestive enzymes • hormones
- 9. Exocrine Function pancreatic duct common bile duct ampulla pancreatic enzymes TAIL BODY HEAD UNCINATE
- 10. Aetiology
- 11. Aetiology • Idiopathic • Congenital/ Genetic • Nutritional Deficiency/excess • Traumatic • Infections /Infestation • Autoimmune • Neoplastic (Benign/Malignant) • Degenerative • Iatrogenic • Psychosomatic • Poisoing/ Toxins/ Drug induced..
- 12. Aetiology • Biliary tract disease • Alcohol • Endoscopic retrograde cholangiopancreatography • Trauma • Drugs • Infection • Hereditary pancreatitis • Hypercalcemia • Developmental abnormalities of pancreas • Hypertriglyceridemia • Tumors • Toxins • Surgical procedures • Vascular abnormalities • Autoimmune pancreatitis
- 14. • Cholelithiasis • Ethanol abuse • Idiopathic • Medications • Hyperlipidemia • ERCP • Trauma • Pancreas divisum • Hereditary • Hypercalcemia • Viral infections – Mumps – Coxsackievirus • End-stage renal failure • Penetrating peptic ulcer Acute Pancreatitis Associated Conditions
- 15. Pathophysiology
- 16. Acute Pancreatitis: Pathophysiology • Localized destruction in the pancreas and systemic inflammatory response. • The inciting event is the premature activation of trypsinogen to trypsin within the acinar cell as opposed to in the duct lumen. • It is postulated that this can be caused by elevated ductal pressures (such as in duct obstruction) as well as problems with calcium homeostasis and pH.
- 17. Acute Pancreatitis: Pathophysiology • Early activation of these zymogens leads to localized tissue damage and release of Damage Associated Molecular Patterns (DAMPs) • Lead to increase capillary permeability and damage of endothelium with microvascular thrombosis that causes multiorgan dysfunction syndrome (MODS), the main cause of morbidity and mortality in acute pancreatitis.
- 18. • STAGE 1: Pancreatic Injury – Edema – Inflammation • STAGE 2: Local Effects – Retroperitoneal edema – Ileus • STAGE 3: Systemic Complications – Hypotension/shock – Metabolic disturbances – Sepsis/organ failure SEVERITY Mild Severe Acute Pancreatitis Pathogenesis
- 19. Protective Measures • COMPARTMENTALIZATION - digestive enzymes are contained within zymogen granules in acinar cells • REMOTE ACTIVATION - digestive enzymes are secreted as inactive proenzymes within the pancreas • PROTEASE INHIBITORS – trypsin inhibitor is secreted along with the proenzymes to suppress any premature enzyme activation • AUTO “SHUT-OFF” – trypsin destroys trypsin in high concentrations
- 21. Clinical Features • Demography • Symptoms • History • Signs • Prognosis • Complications
- 22. Demography
- 23. Demography • Incidence & Prevalence • Geographical distribution. • Race • Age • Sex • Socioeconomic status • Temporal behaviour
- 24. Demography • Incidence of acute pancreatitis ranges between 5 and 80 per 100,000 • Age-related demographics • Alcohol-related - 39 years • Biliary tract–related - 69 years • Trauma-related - 66 years • Drug-induced etiology - 42 years • ERCP-related - 58 years • AIDS-related - 31 years • Vasculitis-related - 36 years
- 25. Demography • Generally, acute pancreatitis affects males more often than females. In males, – In males, the etiology is more often related to alcohol – in females, it is more often related to biliary tract disease. – Idiopathic pancreatitis has no clear predilection for either sex.
- 26. Demography • Race-related demographics • 3 to 4 times higher for blacks than whites.
- 27. Demography • Overall, the frequency of acute pancreatitis has been noted to be rising in the United States and the rest of the world. • Whether this trend is related to a true increase in incidence or simply increased detection is difficult to determine.
- 28. Symptoms
- 29. Symptoms • Abdominal pain – Dull, – Boring, and steady; usually sudden in onset and gradually becoming more severe until reaching a constant ache – In the upper abdomen and may radiate directly through to the back – Discomfort frequently improves with the patient sitting up and bending forward. • Nausea and vomiting, sometimes with anorexia • Diarrhea • Fever
- 30. History • Similar complaints • Recent operative or other invasive procedures • Family history of hypertriglyceridemia • Previous biliary colic and binge alcohol consumption (major causes of acute pancreatitis)
- 31. Signs
- 32. Signs • Fever • Tachycardia • hypotension • Abdominal tenderness, muscular guarding distention diminished or absent bowel sounds • Jaundice • Dyspnea tachypnea; basilar rales, especially in the left lung
- 33. Signs • In severe cases, hemodynamic instability and hematemesis or melena • Occasionally, extremity muscular spasms secondary to hypocalcemia Uncommon- • Cullen sign • Grey-Turner sign • Erythematous skin nodules
- 34. Grey-Turner sign
- 35. Cullen sign
- 36. Prognosis
- 37. Prognosis • The mortality in mild acute pancreatitis is less than 1% • The mortality in severe acute pancreatitis is 10%-15%. • Patients with biliary pancreatitis tend to have a higher mortality than patients with alcoholic pancreatitis. • In patients with severe disease (organ failure), who account for about 20% of presentations, mortality is approximately 30%.
- 38. Complications
- 40. Systemic Compilcations • Cardiovascular: hypotension,Arrhythmias • Pulmonary: pleural effusions, ARDS • Renal: acute tubular necrosis • Hematologic: disseminated intravascular coag. • Metabolic: hypocalcemia, hyperglycemia,Hyperlipidemia • GI: ileus, hemorrhage • Purtscher retinopathy causing temporary or permanent blindness.
- 41. Local Compilcations • Acute fluid collections • Pancreatic necrosis • Pseudocyst • Ascites • Portal/Splenic vein thrombosis • Pseudoaneurysm • Pancreatic abscess / Infected necrosis
- 42. Classification:Predictors of Severity • Why are they needed? – appropriate patient triage & therapy – compare results of studies of the impact of therapy • When are they needed? – optimally, within first 24 hours (damage control must begin early) • Which is best?
- 43. Severity Scoring Systems • Ranson and Glasgow Criteria (1974) – based on clinical & laboratory parameters – scored in first 24-48 hours of admission – poor positive predictors (better negative predictors) • APACHE Scoring System – can yield a score in first 24 hours – APACHE II suffers from poor positive predictive value – APACHE III is better at mortality prediction at > 24 hours • Computed Tomography Severity Index – much better diagnostic and predictive tool – optimally useful at 48-96 hours after symptom onset
- 44. CT Severity Index appearance normal enlarged inflamed 1 fluid collection 2 or more collections grade A B C D E score 0 1 2 3 4 necrosis none < 33% 33-50% > 50% score 0 2 4 6 score morbidity mortality 1-2 4% 0% 7-10 92% 17% Balthazar et al. Radiology 1990.
- 45. Ranson Criteria Alcoholic Pancreatitis AT ADMISSION 1. Age > 55 years 2. WBC > 16,000 3. Glucose > 200 4. LDH > 350 IU/L 5. AST > 250 IU/L WITHIN 48 HOURS 1. HCT drop > 10 2. BUN > 5 3. Arterial PO2 < 60 mm Hg 4. Base deficit > 4 mEq/L 5. Serum Ca < 8 6. Fluid sequestration > 6L Number Mortality <2 1% 3-4 16% 5-6 40% 7-8 100%
- 46. Glasgow Criteria Non-alcoholic Pancreatitis 1. WBC > 15,000 2. Glucose > 180 3. BUN > 16 4. Arterial PO2 < 60 mm Hg 5. Ca < 8 6. Albumin < 3.2 7. LDH > 600 U/L 8. AST or ALT > 200 U/L
- 47. Atlanta classification • Acute pancreatitis is broadly classified as either mild or severe
- 48. Atlanta classification Severe Acute Pancreatitis • Scoring systems – 3 Ranson criteria – 8 APACHE II points – 5 CT points • Organ failure – Shock (SBP < 90 mmhg) – Pulmonary edema / ARDS (pao2 < 60 mmhg) – Renal failure (cr > 2.0 mg/dl) • Local complications – Fluid collections pseudocysts – Necrosis (mortality 15% if sterile, 30-35% if infected) – Abscess
- 49. Investigations •
- 50. Investigations • Laboratory Studies – Routine – Special • Imaging Studies • Tissue diagnosis – Cytology • FNAC – Histology • Diagnostic Laparotomy.
- 51. Diagnostic Studies Imaging Studies • X-Ray • USG • CT • Angiography • MRI • Endoscopy • Nuclear scan
- 53. Laboratory Studies • Serum amylase and lipase • Liver-associated enzymes • Blood urea nitrogen (BUN), creatinine, and electrolytes • Blood glucose • Serum cholesterol and triglyceride • Complete blood count (CBC) and hematocrit; NLR • C-reactive protein (CRP) • Arterial blood gas values • Serum lactic dehydrogenase (LDH) and bicarbonate • Immunoglobulin G4 (IgG4): elevated in autoimmune pancreatitis
- 54. Imaging Studies
- 55. Imaging Studies • Diagnostic imaging is unnecessary in most cases • When the diagnosis is in doubt, • When pancreatitis is severe, • When a given study might provide specific information required
- 56. Imaging Studies • Xray- To exclude du perforation, Pleural effusion • USG- To detedct Gall Stones • CECT- In Severe cases. • MRI- MRCP • Endoscopy ERCP, EUS • CT-guided or EUS-guided aspiration and drainage • Genetic testing
- 57. Acute Pancreatitis Differential Diagnosis • Choledocholithiasis • Perforated ulcer • Mesenteric ischemia • Intestinal obstruction • Ectopic pregnancy • Peptic ulcer disease • Cholangitis • Cholecystitis • Bowel perforation • • • Mesenteric ischemia • Acute hepatitis • Diabetic ketoacidosis • Basilar pneumonia • Myocardial infarction • Renal colic • Aortic dissection
- 59. • Symptoms – Abdominal pain • Laboratory – Elevated amylase or lipase • > 3x upper limits of normal • Radiology – Abnormal sonogram or CT Acute Pancreatitis Diagnosis
- 60. Causes of Increased Serum Pancreatic Enzymes Amylase Lipase Pancreatitis ↑ ↑ Parotitis ↑ Normal Biliary stone ↑ ↑ Intestinal injury ↑ ↑ Tubo-ovarian disease ↑ Normal Renal failure ↑ ↑ Macroamylasemia ↑ Normal
- 61. Management
- 62. Management • Analgesics • Fluid resuscitation • Nutritional support
- 64. Goals of Treatment • Limit systemic injury – support and resuscitation – effective – decrease pancreatic secretion – ineffective / harmful? – inhibit inflammatory mediators – ineffective – inhibit circulating trypsin – ineffective (too late) – removing gallstones – mostly ineffective • Prevent necrosis – how? • Prevent infection – antibiotics (imipenem and ciprofloxacin) – probably effective in necrotic pancreatitis – prevent colonic bacterial translocation – removing gallstones – variably effective • Identify and treat complications
- 65. Treatment of Mild Pancreatitis • Pancreatic rest • Supportive care – fluid resuscitation – watch BP and urine output – pain control – NG tubes and H2 blockers or PPIs are usually not helpful • Refeeding (usually 3 to 7 days) – bowel sounds present – patient is hungry – nearly pain-free (off IV narcotics) – amylase & lipase not very useful here
- 66. Treatment of Severe Pancreatitis • Pancreatic rest & supportive care – Fluid resuscitation* – may require 5-10 liters/day – Careful pulmonary & renal monitoring – ICU – Maintain hematocrit of 26-30% – Pain control – PCA pump – Correct electrolyte derangements (K+, ca++, mg++) • Rule-out necrosis – CECT in 2nd week. – Prophylactic antibiotics if present – Surgical debridement if infected • Nutritional support – May be NPO for weeks – TPN vs. Enteral support (ten)nasojujunal feeding.
- 67. Role of ERCP • Gallstone pancreatitis – Cholangitis – Obstructive jaundice • Recurrent acute pancreatitis – Structural abnormalities – Neoplasm – Bile sampling for microlithiasis • Sphincterotomy in patients not suitable for cholecystectomy
- 68. Enteral Nutrition in Severe Pancreatitis • May start as early as possible – When emesis has resolved – Ileus is not present • Nasojejunal route preferred over nasoduodenal • Likely decreases risk of infectious complications by reducing transmigration of colonic bacteria
- 69. Antibiotics • Antibiotics (usually of the imipenem class) should be used in any case of pancreatitis complicated by infected pancreatic necrosis but should not be given routinely for fever, especially early in the presentation • Antibiotic prophylaxis in severe pancreatitis is controversial; routine use of antibiotics as prophylaxis against infection in severe acute pancreatitis is not currently recommended
- 71. Operative Therapy • Gallstone pancreatitis: Cholecystectomy • Pancreatic duct disruption: Image-guided percutaneous placement of a drainage tube into the fluid collection • Stent or tube placement via ERCP • In refractory cases, distal pancreatectomy or a whipple procedure • Pseudocysts:
- 72. Operative Therapy • Pseudocysts: – None necessary in most cases; – For large or symptomatic pseudocysts, • Percutaneous aspiration • Endoscopic transpapillary or transmural techniques • Surgical management • Infected pancreatic necrosis: Image-guided aspiration; necrosectomy • Pancreatic abscess: Percutaneous catheter drainage and antibiotics; if no response, surgical debridement and drainage
- 73. Prevention
- 74. Prevention • Screening • Risk reduction
- 75. Prevention • Avoid alcohol • Avoid fatty meals • Prevent Abd trauma. • In gallstone pancreatitis, early cholecystectomy is strongly recommended. • In the setting of hypertriglyceridemia, the goal of specific treatment is to bring down and maintain triglyceride levels to less than 500 mg/dL.
- 76. Guidelines •
- 77. Guidelines • ACG Guidelines 2013, the American College of Gastroenterology (ACG) issued guidelines for the management of acute pancreatitis • AGA Guidelines 2018 AGA guidelines (initial AP management) • WSES Guidelines In June 2019, the World Society of Emergency Surgery (WSES) released updated guidelines for the management of severe acute pancreatitis.
- 78. ConclusionsTake home messages • Acute pancreatitis is a self-limited disease in which most cases are mild. • Gallstones and alcohol are the leading causes of acute pancreatitis. • Abdominal pain with S.Amylase S.Lipase raised >3 times is diagnostic. • CECT is usually not required. If needed do in 2nd week. • Treatment is Agressive fluid resuscitation, analgesia and early enteral feeding.
- 79. ConclusionsTake home messages • PPIs are not indicated. • Antibiotics are not indicated. • Octreotide is not indicated.
- 80. Webinar • >Raised amylase lipase 3 times. • Abd. Pain • Atlanta Classification 2012 • Apache score • Obsolete terms hemorrhagic pancreatitis, • Amylase lipase has no severity correlation, prognosis- no serial monitoring. • CT no need if diagnosis is clear . Do it 2nd week..
- 81. Webinar • CT Eevaluatioon of complications, severity • CT severity grades. • Modified severity index. • MRI if contrast allerrgy • TT- no role of colloids. Give RL 20ml.kg bolus 3ml/kg/hour watch ivc diameter/ cvp • Respiratory support. • Pain conntrol NSAIDs, Tramodol, Narcotics • Eearly enteral feeding nasojejunal tube
- 82. Webinar • ERCP – cholangitis, bile duct obstruction • Surgery • Compartment syndrome >20mm of mercury • No necrosectomy
- 83. Lessons From Criticon 2022 D Nageshwar Reddy on acute pancreatitis in ICU- • Cause of death Infected necrosis organ failure SIRS • Modified Marshall score • Elderly • Comorbidity obesity • BUN is a good predictor of severity • Aggressive fluid therapy RL/NS use USG to monitor.
- 84. D Nageshwar Reddy • Early enteral feeding prevents infection • Low fat solid diet. Oral or tube. • Avoidance of prophylactic antibiotics • TARGET 0.5- 1 ML urine output • MAP 65 TO 85 • No benefit of Rules tube • No benefit of Foley catheter • Early ERCP if cholangitis (raised SGOT, SGPT.) • Don't use PPIs.
- 85. Modified Marshall Organ Failure Score • Organ system Score 0* Score 1 Score 2 Score 3 Score 4 Cardiovasc ular (systolic blood pressure)† > 90 mm Hg < 90 mm Hg (fluid responsive) < 90 mm Hg (not fluid responsive) < 90 mm Hg (pH < 7.3) < 90 mm Hg (pH < 7.2) Renal (serum creatinine) ‡ < 1.4 mg/dL (≤ 134 micromol/L ) 1.4–1.8 mg/dL (134–169 micromol/L ) 1.9–3.6 mg/dL (170–310 micromol/L ) 3.6–4.9 mg/dL (311–439 micromol/L ) > 4.9 mg/dL (> 439 micromol/L ) Respiratory (PaO2/FiO 2)§ > 400 mm Hg 301–400 mm Hg 201–300 mm Hg 101–200 mm Hg ≤ 101 mm Hg
- 86. MCQs
- 87. MCQs • Which of the following is the most common cause of acute pancreatitis? A.Alcoholism B.Gallstones C.Smoking D.Viral infection
- 88. MCQs • Which of the following is the most common cause of acute pancreatitis? A.Alcoholism B.Gallstones C.Smoking D.Viral infection
- 89. MCQs • Which of the following tests has a sensitivity and specificity of > 90% for acute pancreatitis? A.Amylase:creatinine clearance ratio test B.Serum amylase level C.Serum lipase level D.Urine trypsinogen-2 dipstick test
- 90. MCQs • Which of the following tests has a sensitivity and specificity of > 90% for acute pancreatitis? A.Amylase:creatinine clearance ratio test B.Serum amylase level C.Serum lipase level D.Urine trypsinogen-2 dipstick test
- 91. MCQs • Basic treatment of acute pancreatitis includes early fluid resuscitation, analgesia, and which of the following? A.Antibiotics B.Endoscopic retrograde cholangiopancreatography (ERCP) C.Enteral nutrition D.Total parenteral nutrition
- 92. MCQs • Basic treatment of acute pancreatitis includes early fluid resuscitation, analgesia, and which of the following? A.Antibiotics B.Endoscopic retrograde cholangiopancreatography (ERCP) C.Enteral nutrition D.Total parenteral nutrition
- 93. MCQs • Basic treatment of acute pancreatitis includes early fluid resuscitation, analgesia, and which of the following? A.Antibiotics B.Endoscopic retrograde cholangiopancreatography (ERCP) C.Enteral nutrition D.Total parenteral nutrition
- 94. MCQs • Which of the following physical findings may indicate severe necrotizing pancreatitis? A. Jaundice B. Erythematous skin nodules C. Fever D. Hypotension
- 95. MCQs • Which of the following physical findings may indicate severe necrotizing pancreatitis? A. Jaundice B. Erythematous skin nodules C. Fever D. Hypotension
- 96. MCQs • Which of these findings is the most common in acute pancreatitis? A. Distention B. Jaundice C. Dyspnea D. Hematemesis
- 97. MCQs • Which of these findings is the most common in acute pancreatitis? A. Distention B. Jaundice C. Dyspnea D. Hematemesis
- 98. MCQs • Which of the following is accurate about the workup of patients with suspected acute pancreatitis? A. Aggressive hydration is rarely necessary B. Contrast-enhanced CT scanning and/or MRI should be performed in all cases C. Routine use of prophylactic antibiotics is indicated D. Intervention in patients with infected necrosis may be delayed through the use of antibiotics that do not penetrate the necrotic tissue
- 99. MCQs • Which of the following is accurate about the workup of patients with suspected acute pancreatitis? A. Aggressive hydration is rarely necessary B. Contrast-enhanced CT scanning and/or MRI should be performed in all cases C. Routine use of prophylactic antibiotics is indicated D. Intervention in patients with infected necrosis may be delayed through the use of antibiotics that do not penetrate the necrotic tissue
- 100. MCQs • Which of the following should not be used in the short term in patients suspected of having autoimmune pancreatitis who present with acute pancreatitis? A. Corticosteroids B. Analgesics C. Enteral feeding D. Mechanical ventilation
- 101. MCQs • Which of the following should not be used in the short term in patients suspected of having autoimmune pancreatitis who present with acute pancreatitis? A. Corticosteroids B. Analgesics C. Enteral feeding D. Mechanical ventilation
- 103. Get this ppt in mobile 1. Download Microsoft PowerPoint from play store. 2. Open Google assistant 3. Open Google lens. 4. Scan qr code from next slide.
- 104. Get this ppt in mobile
- 105. Get my ppt collection • https://www.slideshare.net/drpradeeppande/ edit_my_uploads • https://www.dropbox.com/sh/x600md3cvj8 5woy/AACVMHuQtvHvl_K8ehc3ltkEa?dl =0 • https://www.facebook.com/doctorpradeeppa nde/?ref=pages_you_manage
Editor's Notes
- https://www.ncbi.nlm.nih.gov/books/NBK482468/ drpradeeppande@gmail.com 7697305442
- https://emedicine.medscape.com/article/181364-overview
- Here are the details…
- Here are the details…
- The pancreas lies in the retroperitoneum nestled in the C-loop of the duodenum and posterior to the stomach. Physiologic function of the pancreas. The human pancreas has three general functions: (1) neutralizing the acid chyme entering the duodenum from the stomach; (2) synthesis and secretion of digestive enzymes after a meal; and (3) systemic release of hormones that modulate metabolism of carbohydrates, proteins, and lipids.
- To understand pancreatitis, you need a basic understanding of pancreatic exocrine function
- Three stages of pathophysiology of acute pancreatitis The pathophysiology of acute pancreatitis can be considered as involving three stages. The first stage is pancreatic injury with edema, inflammation, necrosis of pancreatic fat, and variable degrees of necrosis of pancreatic secretory cells. The second stage is spread of the inflammatory process to surrounding tissues, with development of retroperitoneal edema, peripancreatic fat necrosis, and an ileus, with ;third spacing; of fluid and electrolytes in the gastrointestinal tract resulting in hemoconcentration (increased hematocrit). The third stage involves systemic complications, such as hypotension/shock, multiorgan system failure (eg, respiratory, renal), metabolic disturbances, such as hypoalbuminemia and hypocalcemia, and sepsis.
- Resent data has curbed some of the excitement re: use of APACHE in early pancreatitis. In short, prediction of severity is sub optimal at the present time.
- So, even if we can’t identify severe cases sooner, the CT index appears to be the best way to judge severity.
- intestinal decontamination study – no improvement
- mild panc – support is all that’s needed hypotension probably predisposes to necrosis (poor microcirculation)
- *common serious error to underestimate volume needs may need SG catheter – lookout for ARF or ARDS we have impacted the early mortality by better support…late mortality still problem
