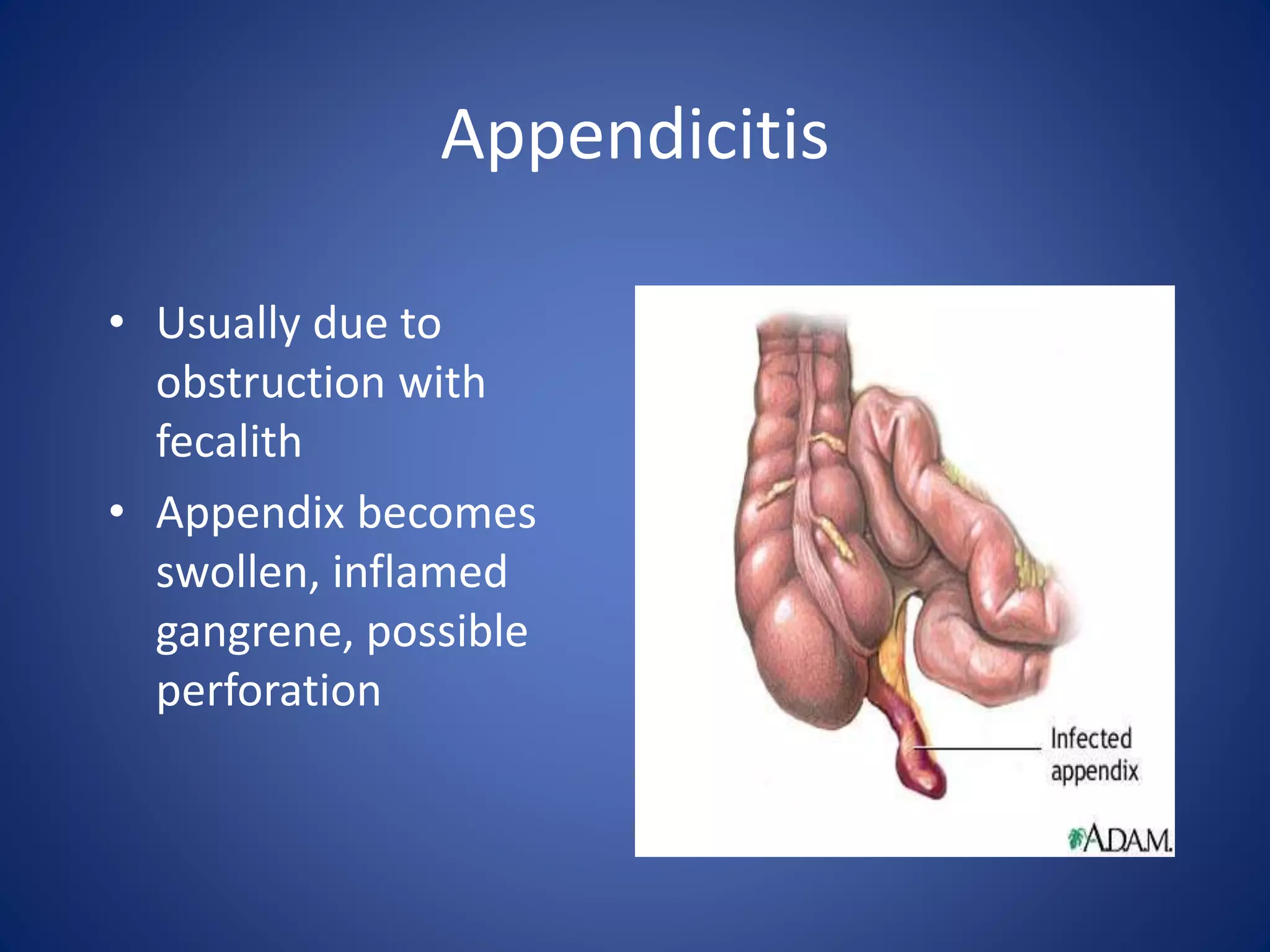
The document discusses the evaluation and management of acute abdominal pain. It describes how acute abdominal pain can be caused by many different intra-abdominal and extra-abdominal conditions ranging from minor to life-threatening. A thorough history, physical exam, and diagnostic testing are needed to make an accurate diagnosis as the cause is often not apparent initially. Common etiologies of acute abdominal pain discussed include appendicitis, cholecystitis, diverticulitis, pancreatitis, bowel obstruction, renal colic, pelvic inflammatory disease, and ectopic pregnancy.