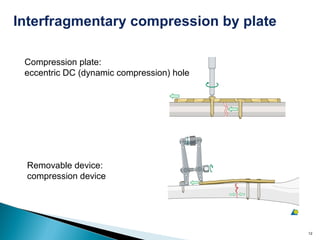
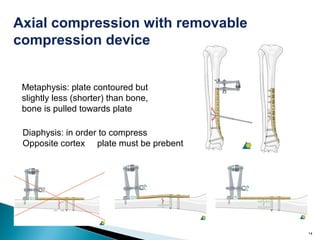
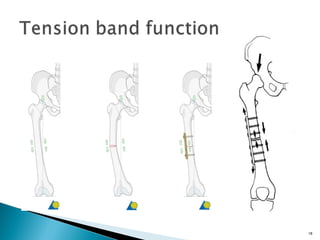
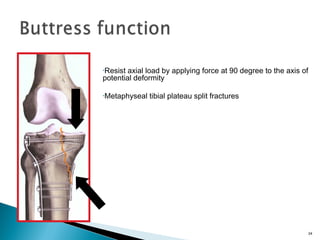
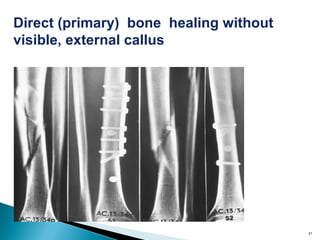
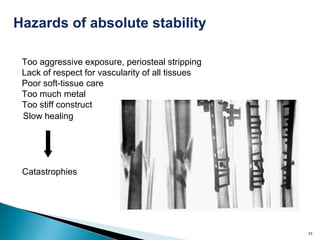
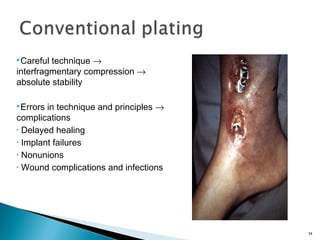
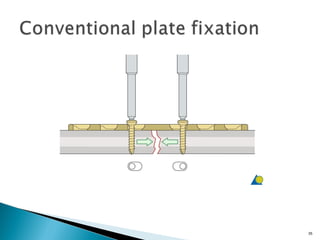
1) Different types of plates function to produce absolute stability through interfragmentary compression, including compression plates, tension band plates, and buttress plates.
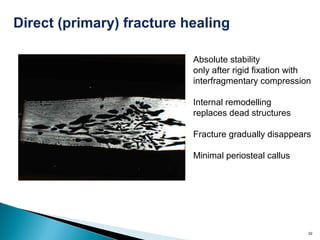
2) Absolute stability is achieved when fracture surfaces do not displace under functional loads, which requires neutralizing all forces through interfragmentary compression.
3) The key to absolute stability is using lag screws in combination with plates to provide interfragmentary compression between fracture fragments.

![ Compression must sufficiently neutralize all
forces[bending, tension, shear and rotation]
6](https://image.slidesharecdn.com/absolutestabilityplatefixfin-140313051328-phpapp01/85/Absolute-stability-plate-fixation-6-320.jpg)
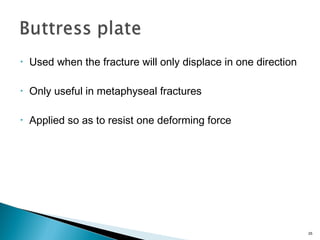
![• Neutralization[Protection] plate
• Compression plate
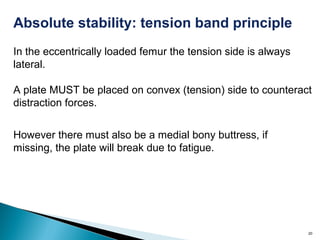
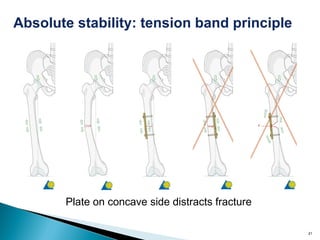
• Tension band plate
• Buttress plate
• Bridge plate—relative stability
8](https://image.slidesharecdn.com/absolutestabilityplatefixfin-140313051328-phpapp01/85/Absolute-stability-plate-fixation-8-320.jpg)