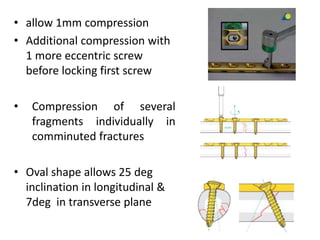
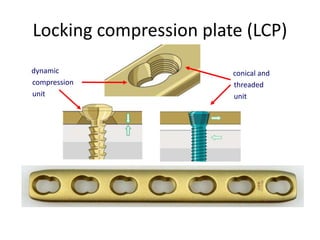
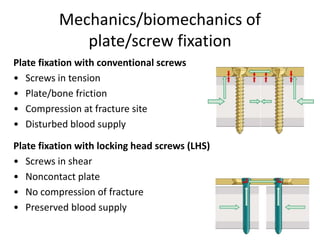
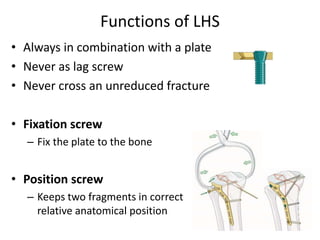
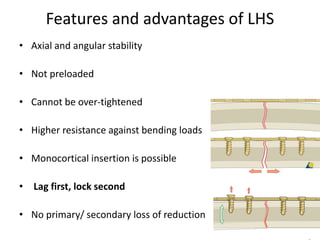
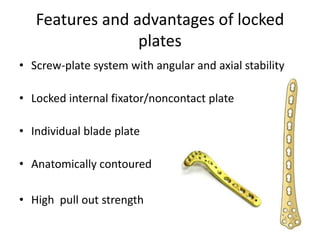
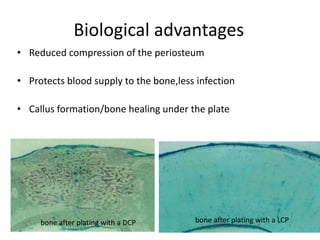
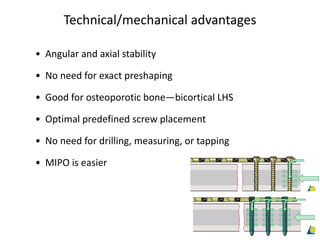
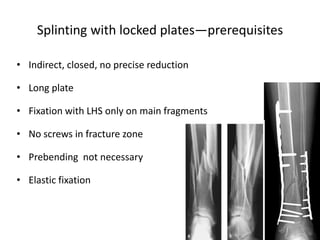
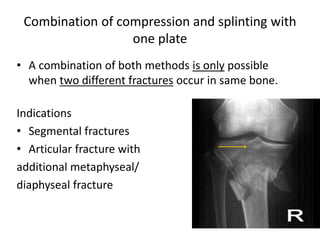
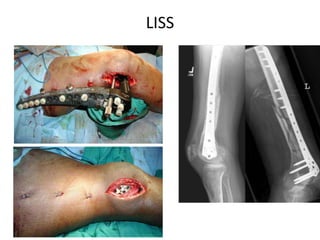
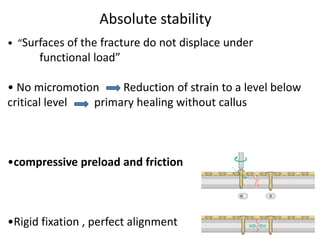
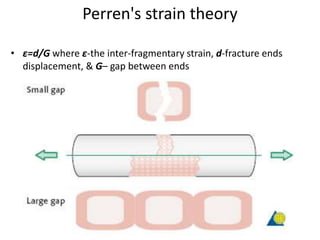
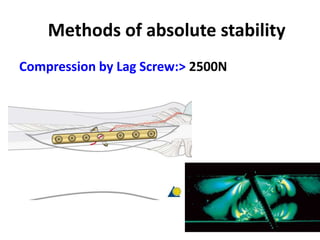
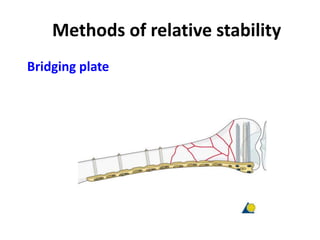
This document discusses the principles of absolute and relative stability in fracture fixation, as well as locking compression plates. It describes how absolute stability aims to reduce strain below a critical level for primary healing without callus formation, while relative stability allows some motion and secondary bone healing through callus formation. Locking compression plates provide angular stability through locking head screws in the plate and bone, maintaining blood supply while providing fixation. They can be used for compression of reduced fractures or for splinting in multifragmentary fractures.




![Plate function
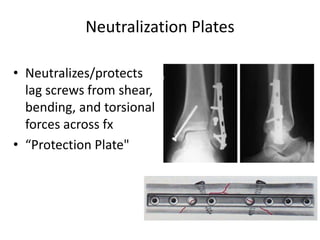
• Neutralization[Protection] plate
• Compression plate
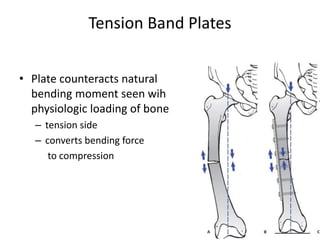
• Tension band plate
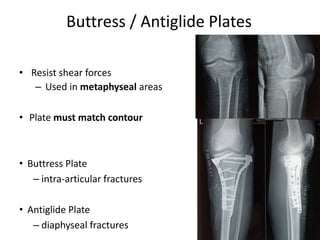
• Buttress plate
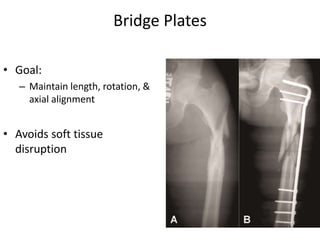
• Bridge plate
14](https://image.slidesharecdn.com/principlesoflockingcompressionplates-200727174943/85/Principles-of-locking-compression-plates-14-320.jpg)