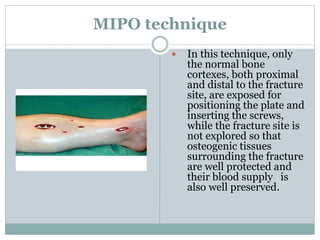
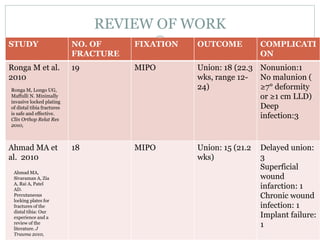
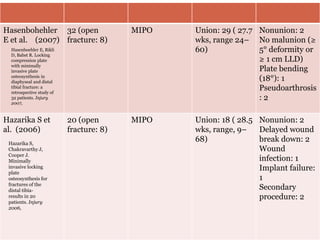
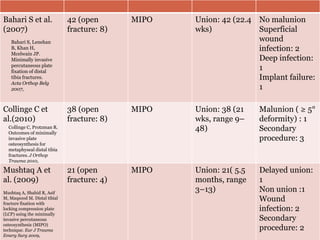
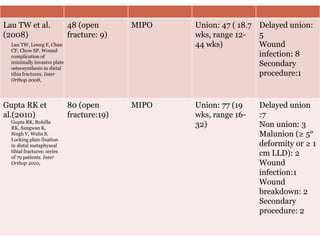
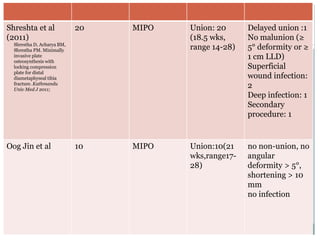
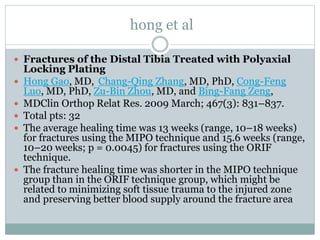
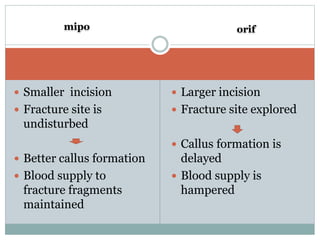
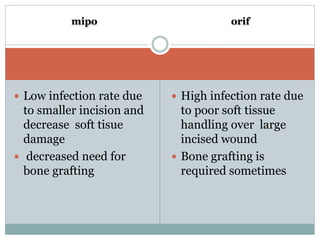
This document discusses outcomes of treating distal tibia fractures using minimally invasive plate osteosynthesis (MIPO) technique. It provides an overview of the MIPO surgical procedure and reviews several studies comparing MIPO to traditional open reduction and internal fixation. The studies found MIPO resulted in high union rates, shorter healing times, and fewer complications like infection compared to open reduction. MIPO preserves the fracture site's blood supply and limits soft tissue damage, allowing for better callus formation and healing.