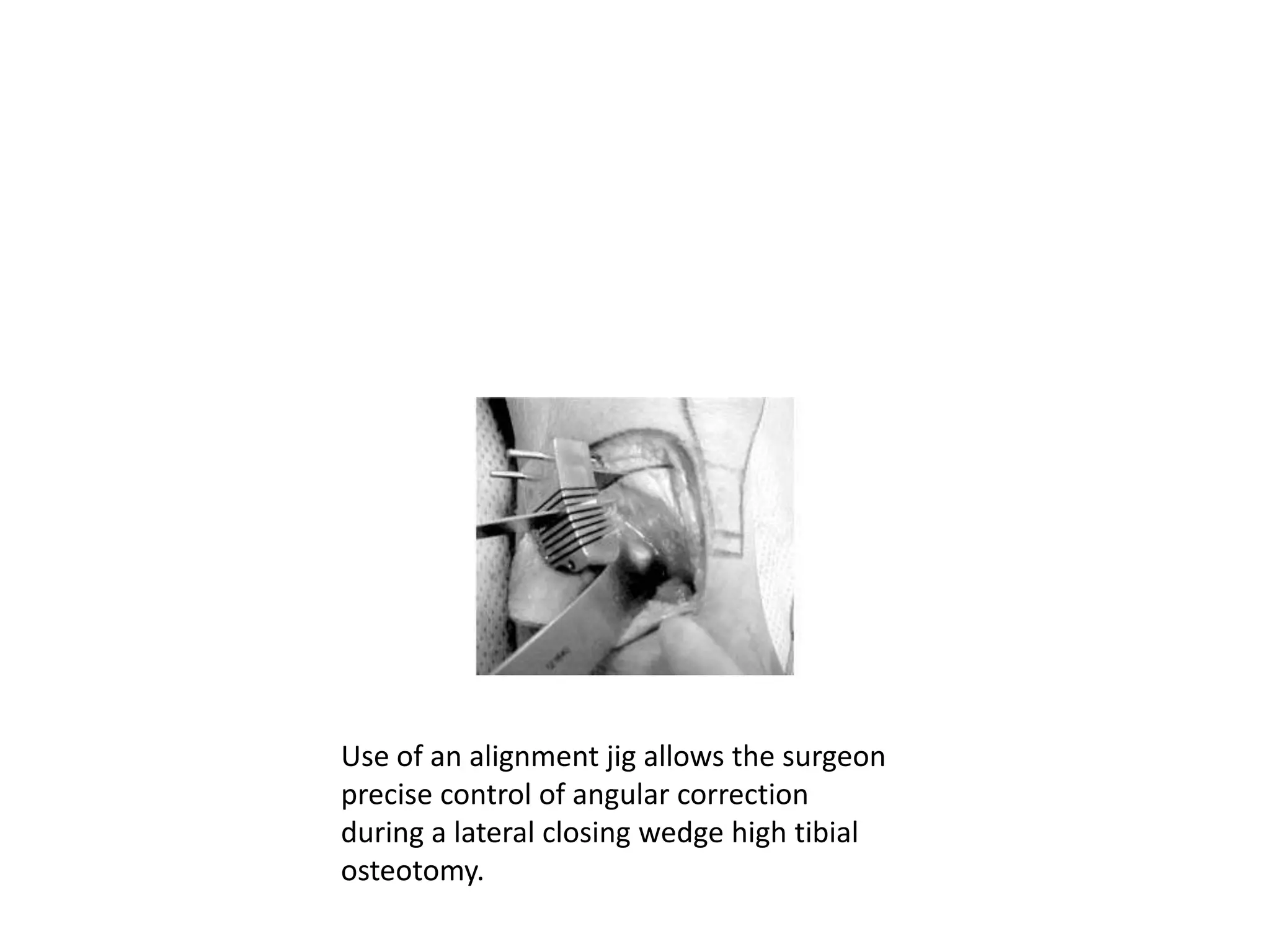
High tibial osteotomy (HTO) is a surgical procedure that involves correcting angular deformities of the tibia. It has been used to treat conditions like osteoarthritis, osteochondritis dissecans, and malalignment. There are several techniques for HTO including lateral closing wedge osteotomy, medial opening wedge osteotomy, and dome osteotomy. HTO can help relieve pain from unicompartmental osteoarthritis and delay the need for knee replacement in young, active patients. Potential complications include fracture, nonunion, nerve palsy, and issues that can make later knee replacement more difficult. Precise surgical planning and fixation are important for achieving good outcomes from HTO.